WEBINAR: Paging Dr. Burnout: Why Technology Should Improve, Not Impede, Physician Experience and Patient Care
Although many provider organizations, physicians, and health plans see the value in moving from fee-for-service to value-based care, the problem can’t be solved by technology alone. Often, it is not only a technology problem – it’s a clinical workflow problem. The result of current practices is an alarming rate of physician burnout. Although government regulations and industry experts weigh in on the importance of both value-based care and interoperability separately, the two are interdependent. Electronic health records were made to improve healthcare, not impede it. Healthcare IT execs and physicians should work smarter, not harder, to solve for interoperability, exchange of data, and ease of use of electronic health records all in the name of reaching value-based care adoption and improving patient lives.
Why the Data Matters
A new survey reveals only 37% of payers and 58% of healthcare providers are very confident that their member/patient demographic information is correct. Having the most up-to-do date patient data within the EMR for pre-and post-visit encounters helps ensure accuracy and timely delivery of needed information. Accurate and up-to-date data, embedded in the clinical workflow and EMR at the point of care, improves physician experience and reduces administrative burden to help ensure revenue integrity.
Why Timing Matters
When it comes to capturing revenue and coding claims after a clinical encounter, timing matters. Having clinical decision support that can deliver clinical activity summaries in days not months will accelerate the move from fee-for-service to value-based care.
Why Communication Matters
Many health plans cite payer-provider communication as a primary barrier to accurate claims and in closing care gaps. It is critical to provide patient data directly within the physician’s preferred clinical workflow (inside the EMR) to enhance adoption and clinical action by surfacing key payer insights and data into a closed loop workflow.
Speakers:

Dr. Matt Lambert
Chief Medical Officer
Curation Health
Dr. Matt Lambert brings more than 20 years of experience as a clinician, CMIO, and change leader in value-based care, ensuring that patients receive more comprehensive care and that payers and providers better capture the value of their services. He is a practicing, board-certified emergency medicine provider who previously founded his own physician staffing company.
Dr. Lambert was one of the founding members of Clinovations. During his time there he served as part of the leadership team for several electronic health record implementations at the nation’s largest public health system in New York City, the University of Washington in
Seattle, Johns Hopkins, Barnabas Health, Medstar, and Broward Health. He is also the author off two healthcare books: Unrest Insured and Close to Change: Perspectives on Change and Healthcare for a Doctor, a Town, and a Country.

Steven Waldren
Vice President and Chief Medical Information Officer
American Academy of Family Physicians
Dr. Waldren is a family physician informaticist. He hold a Masters in Health Informatics from the Univ. of Missouri and a Medical Degree from the University of Kansas. He completed his family medicine residency at Wesley Family Medicine in Wichita, KS. In his current role at AAFP, he has increased the adoption of electronic health records in their membership for 10% to 40%+ over a 3 year period; and to over 70% today. He is a subject experts in physician Adoption of technology, health-IT standards, controlled terminology/ontology, health information exchange, health-IT policy, XML messaging and modeling, and clinical decision support.
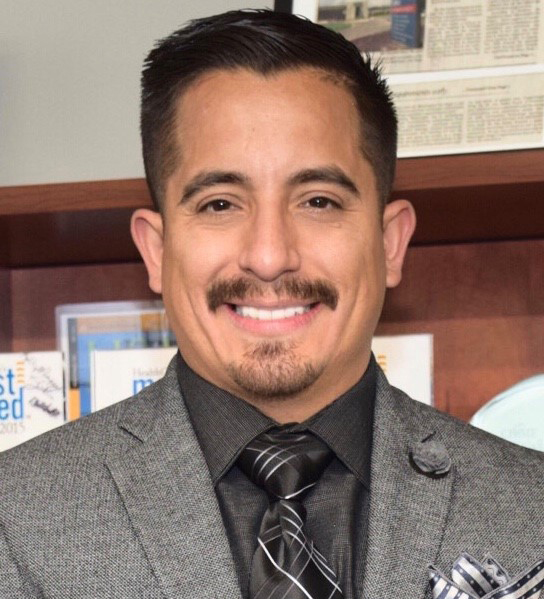
Mike Archuleta
Chief Information Officer
HIPAA & Information Security Officer
Mt. San Rafael Hospital
Recognized as a Top Hospital and Health System CIO to know and named a Rising Star in Healthcare, Michael is a cutting edge, innovative, visionary leader who possesses strong leadership skills with extensive experience and a proven track record of driving increased levels of productivity, profits, high integrity customer relationship skills and expert problem-solving approaches. Michael is an active member of the College of Healthcare Information Management Executives, a technology and cybersecurity advisor to several startups and an active speaker within the field of Health Information Technology.
Under Michael’s guidance and leadership, Mt San Rafael Hospital became one of the leading hospitals in the State of Colorado for leveraging advanced technology to enhance the patient and provider experience. With Michael’s innovative, driven approach, the hospital met HIMSS Analytics Stage Six, a feat only reached by thirty percent of U.S. hospitals. Leveraging advanced Information Technology to improve performance for value-based health care in the areas of infrastructure, business, administrative management, quality, safety, and clinical integration the Information Technology Department has also been presented the 2015, 2016, 2017, 2018, 2019 and 2020 Healthcare’s Most Wired Award which is given annually to the top hospitals in the country making the most progress in the adoption of Health Information Technology.

Jen Covich Bordenick
Chief Executive Officer
eHI
For over 20 years, Jennifer has focused on quality and innovative technology solutions to transform healthcare. As CEO, she provides leadership for research, education and advocacy components of eHealth Initiative and Foundation (eHI). Convening senior executives from every group in healthcare to discuss, identify, and share best practices that transform the delivery of healthcare. Focus areas: improving health and wellness through innovative solutions; interoperability; privacy concerns; artificial intelligence; payment models to support innovative care; and tech tools for chronic care. She led development of dozens of national surveys and published groundbreaking reports. As part of her work with the Foundation, she led grants with California Health Care Foundation, Commonwealth Fund, Aetna Foundation and Bristol Meyers Squibb Foundation. Jennifer is co-chair of the Federal HIT Policy Committee’s Strategy and Innovation Workgroup; member of the HL7 Board of Directors; and a member of the Diabetes Collaborative Stakeholder Panel. Jennifer is a faculty member for the MHA and MHIA graduate programs at George Washington University. Prior to joining eHI, Jennifer headed up the strategic marketing at OpenNetworks, Inc., focusing on security solutions for the healthcare industry. She led healthcare industry relations at MicroStrategy, Inc., focusing on data-mining solutions for the pharmaceutical and healthcare industry. She spent four years at the National Committee for Quality Assurance as Director of Policy and Product Development, helping develop national quality standards for healthcare organizations. Jennifer began her career at the George Washington University Hospital, Medical Center and Health Plan working on quality management initiatives, clinical pathways and healthcare administration. Jennifer earned a master's in Human Resource Development, completed coursework in health administration doctoral program at GWU, and resides in Maryland with her husband and two children.
This webinar is supported by

WEBINAR: The New Era of Healthcare - Patient Engagement and Consumerism
Despite investment in new consumer-facing digital health technologies, health plans and providers still struggle to meaningfully engage vulnerable populations. Join eHI in a discussion with experts to explore how to increase engagement of individuals at risk of worsening physical and mental conditions, including diabetes, social isolation, and injuries from falling. In this webinar, you’ll hear from two panels regarding the various ways that technology can be utilized to target and engage at-risk populations.
Speakers:

Amy McDonough
Managing Director & General Manager
Fitbit Health Solutions at Google
As the Chief Operating Officer for Fitbit Health Solutions, Amy leads the team working with employers, health plans and health systems to design solutions and programs focused on engagement, positive return on investment and health outcomes. Before her COO role, Amy took on several key positions leading Fitbit’s B2B efforts. Prior to Fitbit, Amy held strategic roles at CNET Networks, including Director of Audience and Content Development for the Community Division and Director of Strategic Partnerships for the Network. Amy has a bachelor’s degree from Merrimack College in Andover, MA and a Professional Certificate in Integrated Marketing Communications from the UC Berkeley Extension program.

Stacy Ward-Charlerie, PharmD, MBA
Director, Product Development
Strategy & Growth Department
AllianceRx Walgreens Prime
Stacy Ward-Charlerie is a Clinical Informatics Pharmacist with more than a decade of experience working in product and informatics roles. Currently, she is the Director of Product Development Solutions at AllianceRx Walgreens Prime, one of the nation’s largest specialty pharmacies. In this role she is responsible for leading the development new products and programs for payer and pharma clients. Prior to joining AllianceRx Walgreens Prime, Dr. Ward-Charlerie served as the President of WardRx Consulting, a firm providing consulting services for organizations seeking to use or enhance health information technology to improve clinical outcomes.
Previously, she held various roles at Surescripts, the nation’s largest health information network. While there, she led the growth and innovation of their Medication History product portfolio. She was also instrumental in launching the Critical Performance Improvement Program, working across the Surescripts Network Alliance to improve the quality of e-prescriptions. Dr. Ward-Charlerie spent her early career in the intersection of managed care and informatics working for Kaiser Permanente focusing on EHR system configuration to support utilization/formulary management and quality/safety initiatives.
Dr. Ward-Charlerie has published several peer-reviewed research articles on the interoperable exchange of healthcare data. She has served as an adjunct clinical faculty member at Notre Dame of Maryland University, graduate faculty at George Mason University and precepts PharmD candidates from local universities.
She received a Bachelor of Science degree in Biology from Nova Southwestern University, a Doctor of Pharmacy degree from Howard University College of Pharmacy, and completed a PGY1 residency program with Kaiser Permanente Mid-Atlantic States. She also holds an MBA in Healthcare Management.

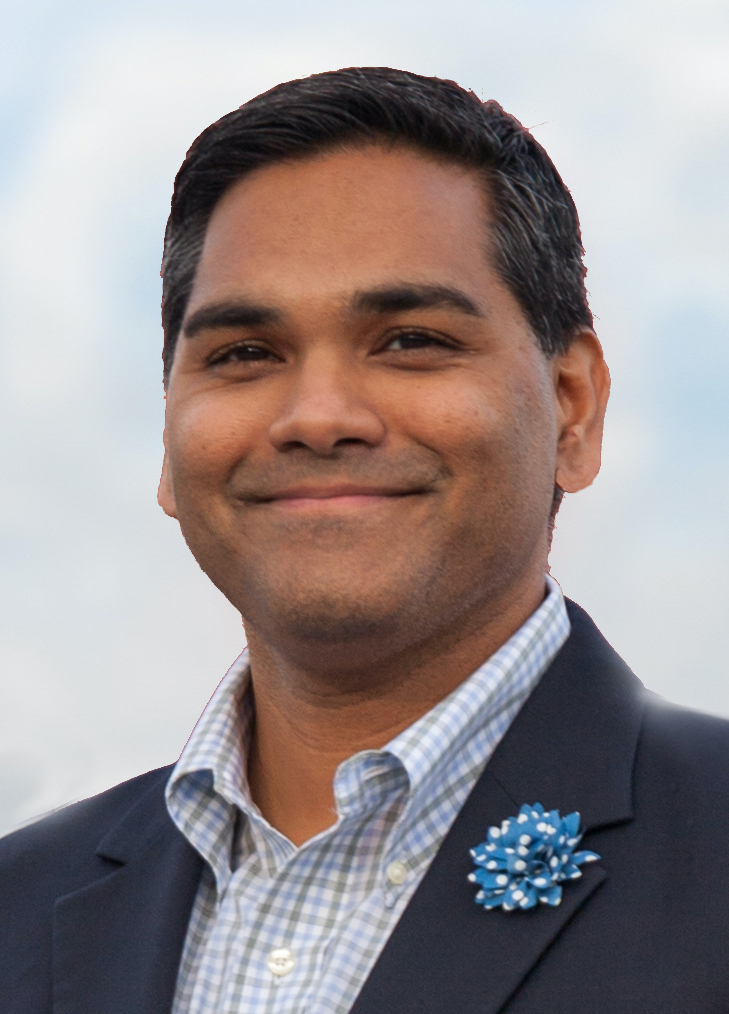
Henry Archibong
Associate Vice President, Innovation Solutions
Inovalon
Mr. Archibong serves as Associate Vice President of Innovation Solutions for Inovalon, leading product innovation, interoperability strategy and operations for the Company’s payer and provider business units, as well as efforts to expand Inovalon’s connectivity infrastructure.
Mr. Archibong has nearly two decades of experience in healthcare IT. He began his career with Johnson & Johnson (J&J), where he successfully streamlined IT project execution and resource management across all 250 J&J operating companies globally.
Mr. Archibong transitioned into healthcare when was tapped to join Cooper University Health Care, in Camden, NJ, as their Director of Enterprise Applications. There, he successfully led the system-wide implementation and adoption of the Epic Electronic Health Record (EHR) for the health system.
He later joined Anne Arundel Medical Center (AAMC) in Annapolis, MD, as their Executive Director and Associate Chief Information Officer (ACIO). There he led several technology advancements for the health system, including the launch of a new Enterprise Resource Planning system, a Picture Archiving and Communication System (PACS), and deployment of Epic EHR across all of their ambulatory clinics. AAMC was recognized as one of the nation’s Most Connected Hospitals by U.S. News and World Report, as well as a HealthCare's Most Wired Hospital in 2015 and 2016 during his tenure as ACIO.
Prior to joining Inovalon, Mr. Archibong served as the Vice President and Site Executive for University of Maryland Capital Region Health in Prince Georges County, MD.

Fred Bentley
Managing Director, Policy
Avalere
Fred Bentley advises clients on health delivery and payment innovation, providing analytic and strategic insight on issues related to the delivery of care.
As an expert in fields ranging from payer strategy to hospital–physician alignment and post-acute care, he has worked with providers, including integrated delivery networks, academic medical centers, post-acute providers, and long-term care organizations as well as national and regional health plans. Over the past 5 years, his work has focused on supporting health systems engage in Medicare and Medicaid payment and delivery system transformation initiatives.
Prior to joining Avalere, Fred was a principal in the Accountable Care Solutions practice at The Chartis Group. In this role, he worked with leading hospitals and health systems in developing strategic roadmaps to guide their clinical innovation, population health, and cross-continuum integration initiatives. He also served as a managing director with The Advisory Board Company, managing a team of consultants and analysts who supported provider organizations ranging from physician groups and health systems to post-acute care providers.
Fred holds an MPP and MPH from the University of California, Berkeley, and a BA in political science from Haverford College.

Hope Kragh
Vice President, Health Plan Solutions
Amwell
For over 30 years, Hope has leveraged her passion and energy to drive her work with employers, health plans, and health systems to manage their enormous investment in healthcare for employees, members and patients. At both large and start-up healthcare companies, Hope created and executed client experience + success strategies, and directly impacted business development and strategic partnership results. She joined Amwell as VP, Health Plan Solutions, in 2020 to lead the company’s strategic work with health plans’ telehealth strategies following several years with start-up Collective Health where she developed the vision, design, and execution of a full-scale client experience team + strategy for a business portfolio spanning multiple segments. Hope’s additional experience spans over 25 years in national health plan carriers such as Anthem, UHC and CIGNA.
Hope has deep knowledge of the healthcare industry overall including network delivery models, population health and employee benefits strategies, plan operations, marketing, analytics, and consumer insights, and contract negotiations. She is passionate about disruptive change that will improve our healthcare delivery system and patient experience + outcomes and has been an active participant in health industry initiatives led by Pacific Business Group on Health, Catalyst for Payment Reform and the Purchaser Value Network Council.
Hope has also been a keynote speaker and expert panelist for healthcare industry events throughout the country, including MedCity Converge Conference, Health2.0, The Conference Board Healthcare Conference, Silicon Valley Employers' Forum Innovation Summit, Collective Create Health Conference, National Sales Meetings, and numerous industry fireside chats.

Eric Sullivan
Senior Vice President, Innovation and Data Strategies
Inovalon
Mr. Sullivan serves as Senior Vice President of Innovation and Data Strategies at Inovalon, supporting the innovation towards new product and technology solutions and providing executive leadership over all data integration, management, and governance programs. For more than 25 years, Mr. Sullivan has been leading clinical innovation and data-driven solutions in a variety of roles in the healthcare sector—with a keen focus on developing data-driven models to transform healthcare by improving quality, outcomes, and efficiency. He has held leadership positions in some of the nation’s largest health plans including UnitedHealthcare and led teams in the clinical care setting to deliver patient-centered, patient specific health care. His current role advances patient-precision analytics by leveraging big data technologies, Natural Language Processing (NLP), interoperability and real-time clinical data patient profiling.
Mr. Sullivan received his M.S. in Health Care Administration as well as an M.B.A from the University of Maryland. Mr. Sullivan also holds a B.S. in Neurobiology from the University of Maryland College Park.

Will Kilbreth
Senior Vice President and Chief Information Officer
Maine Community Health Options
Will has over 20 years of experience in the healthcare, technology, and finance fields. Prior to joining Community Health Options, Will was the Deputy Director for Maine’s Dirigo Health Agency, overseeing technical and financial operations. During this time, Will also served as Acting Deputy Director for the Maine Health Data Organization, the state’s all payer claims database. In other roles he has focused on the delivery of business systems and analytics for local and international clients, including MaineSense, Bowdoin, Reuters, AT&T, and British Telecom. Will has a BA in English Literature and Philosophy from McGill University.

Jen Covich Bordenick
Chief Executive Officer
eHI
For over 20 years, Jennifer has focused on quality and innovative technology solutions to transform healthcare. As CEO, she provides leadership for research, education and advocacy components of eHealth Initiative and Foundation (eHI). Convening senior executives from every group in healthcare to discuss, identify, and share best practices that transform the delivery of healthcare. Focus areas: improving health and wellness through innovative solutions; interoperability; privacy concerns; artificial intelligence; payment models to support innovative care; and tech tools for chronic care. She led development of dozens of national surveys and published groundbreaking reports. As part of her work with the Foundation, she led grants with California Health Care Foundation, Commonwealth Fund, Aetna Foundation and Bristol Meyers Squibb Foundation. Jennifer is co-chair of the Federal HIT Policy Committee’s Strategy and Innovation Workgroup; member of the HL7 Board of Directors; and a member of the Diabetes Collaborative Stakeholder Panel. Jennifer is a faculty member for the MHA and MHIA graduate programs at George Washington University. Prior to joining eHI, Jennifer headed up the strategic marketing at OpenNetworks, Inc., focusing on security solutions for the healthcare industry. She led healthcare industry relations at MicroStrategy, Inc., focusing on data-mining solutions for the pharmaceutical and healthcare industry. She spent four years at the National Committee for Quality Assurance as Director of Policy and Product Development, helping develop national quality standards for healthcare organizations. Jennifer began her career at the George Washington University Hospital, Medical Center and Health Plan working on quality management initiatives, clinical pathways and healthcare administration. Jennifer earned a master's in Human Resource Development, completed coursework in health administration doctoral program at GWU, and resides in Maryland with her husband and two children.
This webinar is supported by

WEBINAR: Vaccination Scheduling, Administration, and Documentation in a Digital World
The COVID-19 pandemic is the first mass vaccination effort in decades and it revealed cracks in our healthcare infrastructure. In the beginning of the vaccine rollout in many states, scheduling websites were unable to handle the traffic and to limit the number of appointments scheduled to the number of vaccine doses available. Most providers had no coordinated waitlist method for ensuring that vaccines did not go to waste, even in the face of no-show appointments. Additionally, everyone is now having to deal with the issue that has plagued parents of school-age children for decades: trying not to misplace the vaccination record.
In this session, we explore how digital technologies (Vaccine Passport and Virtual Front Desk) can help enable a more efficient scheduling process, deliver a touchless patient intake process effortlessly and accurately document the vaccination event, and allow the patient to access his or her vaccination record from any digital device.
This webinar will explore:
- Issues related to digital patient scheduling
- Digital solutions for enabling touchless patient intake
- Strategies for capturing vaccination information automatically for digital proof
Speakers:

Navesh Kandiyil, MD,MBA,FACHE
Vice President, Strategic Accounts
Change Healthcare
Dr. Kandiyil has been with Change Healthcare for five years and is currently the Vice President, Strategic Accounts and Healthcare Revenue Cycle. Prior to being a Physician Executive at both Change and McKesson, he was the Senior Consultant, Business Risk at Deloitte and Touche, the Clinical Document Improvement Specialist and Physician Educator at Precyse.
He was the Chief Medical Officer at International SOS for nearly six years and prior to that, a surgical Resident at both University of Mexico’s Health Science Center and Drexel University College of Medicine. He attended MIT CSAIL and MIT Sloan School of Management, attended medical school at Padmashree Dr. D.Y.Patil Medical College and earned an MBA from Northwestern
Gautam Shah
Vice President, Healthcare Platform and Marketplace
Change Healthcare
In his role as Vice President of Platform and Marketplace at Change Healthcare, Gautam M. Shah, known as “G,” leads the organization’s digital transformation, including overseeing the strategy for Intelligent Healthcare PlatformTM, managing and operating the Change Healthcare Digital Marketplace for APIs and SaaS products, leading involvement in industry-regulatory groups that drive the use of APIs, and incubating Change Healthcare’s Virtual Care Enablement solution. Prior to Change Healthcare, he was an executive-in-residence at the Center for Digital Health Innovation at UC San Francisco, and has held executive, technical, and business leadership positions with Vocera, Apollo Global, Jasper, and Sprint.

Jen Covich Bordenick
Chief Executive Officer
eHI
For over 20 years, Jennifer has focused on quality and innovative technology solutions to transform healthcare. As CEO, she provides leadership for research, education and advocacy components of eHealth Initiative and Foundation (eHI). Convening senior executives from every group in healthcare to discuss, identify, and share best practices that transform the delivery of healthcare. Focus areas: improving health and wellness through innovative solutions; interoperability; privacy concerns; artificial intelligence; payment models to support innovative care; and tech tools for chronic care. She led development of dozens of national surveys and published groundbreaking reports. As part of her work with the Foundation, she led grants with California Health Care Foundation, Commonwealth Fund, Aetna Foundation and Bristol Meyers Squibb Foundation. Jennifer is co-chair of the Federal HIT Policy Committee’s Strategy and Innovation Workgroup; member of the HL7 Board of Directors; and a member of the Diabetes Collaborative Stakeholder Panel. Jennifer is a faculty member for the MHA and MHIA graduate programs at George Washington University. Prior to joining eHI, Jennifer headed up the strategic marketing at OpenNetworks, Inc., focusing on security solutions for the healthcare industry. She led healthcare industry relations at MicroStrategy, Inc., focusing on data-mining solutions for the pharmaceutical and healthcare industry. She spent four years at the National Committee for Quality Assurance as Director of Policy and Product Development, helping develop national quality standards for healthcare organizations. Jennifer began her career at the George Washington University Hospital, Medical Center and Health Plan working on quality management initiatives, clinical pathways and healthcare administration. Jennifer earned a master's in Human Resource Development, completed coursework in health administration doctoral program at GWU, and resides in Maryland with her husband and two children.

Patrick Leonpacher
Business Development and Operations Executive, Connected Consumer Health
Change Healthcare
Patrick Leonpacher is a business development and operations executive for Change Healthcare’s Connected Consumer Health suite, a consumer and financial engagement platform to help healthcare providers acquire and retain new patients. Prior to his current role at Change Healthcare, Patrick held management positions at Nortel, as well as executive roles in several healthcare information technology companies. Patrick received his bachelor’s in business administration from University of Florida and his master’s in computer science from the University of West Florida.
This webinar is supported by:

WEBINAR: How APIs are Changing the Economics of EHR Integration
Leveraging APIs for Cost Savings and Value-Added Services and Capturing the Value of APIs
In this webinar, a panel of subject experts talked about the growth of the electronic health record (EHR) app marketplace, and how providers are working to comply with new regulations using innovative solutions to give patients more control of their data, identify gaps in care, improve provider workflow, reduce clinician burnout, and eliminate costs.
Speakers:

Dr. Srinath Adusumalli, MSc, FACC
Assistant Professor of Clinical Medicine - Perelman School of Medicine
Assistant Chief Medical Information Officer - University of Pennsylvania Health System
Dr. Adusumalli is an Assistant Professor of Clinical Medicine at the Perelman School of Medicine, Assistant Chief Medical Information Officer at the University of Pennsylvania Health System and is a general cardiologist, echocardiographer, and assistant cardiovascular disease fellowship program director with the Division of Cardiovascular Medicine at the Hospital of the University of Pennsylvania. He also serves as a clinical innovation manager for the Nudge Unit and the Acceleration Lab at the Penn Medicine Center for Health Care Innovation.
Dr. Adusumalli spends the majority of his time caring for patients with cardiovascular disease in the clinic, inpatient wards, and cardiac intensive care unit. Outside of his clinical commitments, his interests and work focus on the utilization of health information technology to advance Penn Medicine’s tripartite academic mission of clinical care, education, and research. He is particularly interested in methods of using technology to evaluate and accelerate the adoption of evidence-based healthcare in a manner that is safe for patients and easy for clinicians. He has worked on several projects including developing an opt-out default pathway for cardiac rehabilitation referral, deploying active choice interventions directed at statin prescription within the electronic health record, designing and evaluating methods for clinicians to easily refer advanced heart failure patients for home care programs, and designing new evidence-based electronic reporting systems for cardiovascular procedures.

Aneesh Chopra
CEO
CareJourney
Aneesh Chopra is the President of CareJourney, an open data membership service building a trusted, transparent rating system for physicians, networks, facilities and markets on the move to value. He served as the first U.S. CTO and authored "Innovative State: How New Technologies Can Transform Government.”

John Glaser, PhD
Executive-in-Residence
Harvard Medical School Executive Education
John is an Executive-in-Residence at the Harvard Medical School Executive Education. He is a former senior vice president of Population Health, at Cerner Corporation. Previously he was chief executive officer of Siemens Heath Services. Prior to Siemens, John was chief information officer at Partners HealthCare.
John was the founding chair of the College of Healthcare Information Management Executives (CHIME) and the past-president of the Healthcare Information and Management Systems Society (HIMSS). He is the former Chair of the Global Agenda Council on Digital Health, World Economic Forum. He is former Senior Advisor to the Office of the National Coordinator for Health Information Technology.
John serves on the boards of the Scottsdale Institute, PatientPing, National Committee for Quality Assurance, the American Telemedicine Association, Wellsheet, and Relatient.
John has received numerous industry awards including the John P. Glaser Innovation Award (established by the School of Biomedical Informatics, UTHealth), William B. Stead Thought Leadership Award (American Medical Informatics Association) and the Lifetime Achievement Award (CHIME).
John received his Ph.D. from the University of Minnesota. He has written over 200 articles and three books on the strategic application of IT in health care. He is on the faculty of the Wharton School at the University of Pennsylvania, the UTHealth School of Biomedical Informatics and the Harvard School of Public Health.

Craig Limoli
Chief Executive Officer
Wellsheet
Craig Limoli founded Wellsheet after working at IBM as a strategy consultant in their Watson Health division, where he led regional business development for their flagship care coordination product. After seeing the deficiencies in existing technologies in healthcare, Craig saw an opportunity to create a better experience for physicians. Since Craig left Wharton in 2016 to start Wellsheet, the company has raised over 6.5 million of dollars in funding, created a product proven to vastly accelerate physician workflow, and earned the business of some of the largest health systems in the country

Jen Covich Bordenick
CEO
eHI
For over 20 years, Jennifer has focused on quality and innovative technology solutions to transform healthcare. As CEO, she provides leadership for research, education and advocacy components of eHealth Initiative and Foundation (eHI). Convening senior executives from every group in healthcare to discuss, identify, and share best practices that transform the delivery of healthcare. Focus areas: improving health and wellness through innovative solutions; interoperability; privacy concerns; artificial intelligence; payment models to support innovative care; and tech tools for chronic care. She led development of dozens of national surveys and published groundbreaking reports. As part of her work with the Foundation, she led grants with California Health Care Foundation, Commonwealth Fund, Aetna Foundation and Bristol Meyers Squibb Foundation. Jennifer is co-chair of the Federal HIT Policy Committee’s Strategy and Innovation Workgroup; member of the HL7 Board of Directors; and a member of the Diabetes Collaborative Stakeholder Panel. Jennifer is a faculty member for the MHA and MHIA graduate programs at George Washington University. Prior to joining eHI, Jennifer headed up the strategic marketing at OpenNetworks, Inc., focusing on security solutions for the healthcare industry. She led healthcare industry relations at MicroStrategy, Inc., focusing on data-mining solutions for the pharmaceutical and healthcare industry. She spent four years at the National Committee for Quality Assurance as Director of Policy and Product Development, helping develop national quality standards for healthcare organizations. Jennifer began her career at the George Washington University Hospital, Medical Center and Health Plan working on quality management initiatives, clinical pathways and healthcare administration. Jennifer earned a master's in Human Resource Development, completed coursework in health administration doctoral program at GWU, and resides in Maryland with her husband and two children.
This webinar is supported by 
WEBINAR: Leveraging Benefit Data to Improve Patient Satisfaction at the Point of Care
eHI, in partnership with Surescripts, hosted a 60-minute webinar discussing best practices to improve eligibility, formulary & benefit files to positively impact the point of care. The webinar highlighted the importance of having complete eligibility, formulary and benefit data and showcase the benefits of downstream transactions like real-time benefit check, electronic prior auth and specialty enrollment. The webinar also discussed the implementation of the new NCPDP version 5 standard. Panelists will include stakeholders from leading experts in point-of-care transactions.
Speakers:

Pooja Babbrah
Practice Lead for PBM Services
Point of Care Partners
Pooja Babbrah is a seasoned strategy and product leader focused on healthcare technology. She has spent over two decades leading and growing product strategy teams with her main focus on growing a company's revenue through a well-defined and focused product strategy. Most recently, Pooja is serving as a practice lead for Point-of-Care Partners, a management consulting firm focused on healthcare technology and policy where she has helped to grow revenues of the company over 120% over the past few years. Pooja is currently serving on the National Council for Prescription Drug Programs (NCPDP) Board of Trustees and has led the organizations efforts on developing standards and transactions related to specialty medications. She currently serves on the Investment committee for the Arizona State University Foundation – Women and Philanthropy program and also services on the Water1st International Advisory Council.

Dr. Andrew Mellin
VP, Chief Medical Information Officer
Surescripts
Dr. Mellin is focused on helping the Surescripts Network Alliance improve the patient experience with electronic prescribing and the provider workflow. Trained in internal medicine, he has spent more than two decades working in health information technology at companies including McKesson, RedBrick Health and, most recently, Spok. Before that, Dr. Mellin led the provider engagement team at Allina Health in Minneapolis through an EHR implementation spanning eight hospitals and 60 clinics and worked part-time as a hospitalist in St. Paul for 15 years.

Jen Covich Bordenick
Chief Executive Officer
eHealth Initiative
For over 20 years, Jennifer has focused on quality and innovative technology solutions to transform healthcare. As CEO, she provides leadership for research, education and advocacy components of eHealth Initiative and Foundation (eHI). Convening senior executives from every group in healthcare to discuss, identify, and share best practices that transform the delivery of healthcare. Focus areas: improving health and wellness through innovative solutions; interoperability; privacy concerns; artificial intelligence; payment models to support innovative care; and tech tools for chronic care. She led development of dozens of national surveys and published groundbreaking reports. As part of her work with the Foundation, she led grants with California Health Care Foundation, Commonwealth Fund, Aetna Foundation and Bristol Meyers Squibb Foundation. Jennifer is co-chair of the Federal HIT Policy Committee’s Strategy and Innovation Workgroup; member of the HL7 Board of Directors; and a member of the Diabetes Collaborative Stakeholder Panel. Jennifer is a faculty member for the MHA and MHIA graduate programs at George Washington University. Prior to joining eHI, Jennifer headed up the strategic marketing at OpenNetworks, Inc., focusing on security solutions for the healthcare industry. She led healthcare industry relations at MicroStrategy, Inc., focusing on data-mining solutions for the pharmaceutical and healthcare industry. She spent four years at the National Committee for Quality Assurance as Director of Policy and Product Development, helping develop national quality standards for healthcare organizations. Jennifer began her career at the George Washington University Hospital, Medical Center and Health Plan working on quality management initiatives, clinical pathways and healthcare administration. Jennifer earned a master's in Human Resource Development, completed coursework in health administration doctoral program at GWU, and resides in Maryland with her husband and two children.
This webinar is sponsored by Surescripts. 
WEBINAR: How Providers are Scaling Virtual Care: Best Practices and Lessons Learned from the Leaders
The pandemic reshaped healthcare’s utilization of virtual care. Almost overnight, providers quickly mobilized telehealth programs, reshaped audio-only check-ins, and revamped patient engagement solutions. As healthcare leaders refine and grow these programs over the coming months, our experts detail the strategies and practices to help organizations scale from pilots to enterprise-wide, comprehensive virtual care deployments.
Experts convened to create virtual care experiences where the technology is “invisible” to the patients and providers. In their work together, they were able to scale technology and operations for a home monitoring program to 60,000 patients across regions and conditions – within 12 months.
Topics:
- How to bolster provider and patient adoption and buy-in of telehealth and remote patient monitoring
- Best-in-class strategies for systems integration; data management; and device selection, procurement, and support
- Approaches for frictionless patient engagement, enrollment, and onboarding experiences
- Results from studies assessing the return on investment – including member and clinical satisfaction scores, clinical outcomes, and changes in the utilization of healthcare services
Speakers:

Drew Schiller
CEO
Validic
Drew Schiller co-founded and serves as the Chief Executive Officer and Board Director at Validic, the industry’s leading health data platform and remote patient monitoring technology. A patented technologist, Drew believes that technology will humanize the healthcare experience for patients and care providers. He regularly speaks and writes on a variety of topics, including the future of virtual care and the ROI and personal stories from remote monitoring programs.
Drew’s vision, and the mission of his company Validic, is to improve the quality of human life by building technology that makes personal data actionable. Beyond Validic and in pursuit of that mission, Drew serves on the boards of several advocacy and policy groups, including the Consumer Technology Association, the eHealth Initiative, and the Council for Entrepreneurial Development (CED) in North Carolina.

Angie Stevens
Founder
Virtual Insights
Former Executive Director, Telehealth
Kaiser Permanente
As a leader in Telehealth, and founder of Virtual Insights, LLC, Angie Stevens has a wealth of experience in working with large organizations to transform the way care is delivered using innovative technology. She’s an ambitious executive, pioneering the first national Telehealth Technology Strategy for Kaiser Permanente; serving over 12 million consumers. This exemplifies Angie’s proven professional record of thought leadership and ability to unite diverse resources in support of a common goal.
Angie’s keen ability to distill business objectives into actionable plans is evidenced by her professional experience and executive leadership roles held at large organizations including Kaiser Permanente, McKesson Health Solutions, Universal American Corporation, and the TriZetto Group. Some of her most notable career achievements include leading the design and implementation of the largest national Remote Patient Monitoring System, increasing the operational efficiency of Care Management Nurses by 65% while improving patient clinical outcomes. She also increased the top-line revenue and gross profit of a struggling hosting solution in the Payer market in just 18 months by closing large deals with recurring revenue and improving overall operational efficiency. Her ability to think big picture, while executing at scale, led to her receipt of company and market awards, including Fierce Innovation Award and Digital Edge25.
In the workplace, Angie is best known for her entrepreneurial spirit and mission-driven nature. She believes greater results are achieved through a team effort and enjoys mentoring others. Angie is particularly passionate about enriching the organizational capabilities of businesses while shaping the next generation of leadership. She’s driven by her fundamental belief that all people should have access to high-quality healthcare at an affordable cost.
Angie holds an MBA from the Daniels College of Business at the University of Denver.

Jen Covich Bordenick
CEO
eHealth Initiative and Foundation
For over 20 years, Jennifer has focused on quality and innovative technology solutions to transform healthcare. As CEO, she provides leadership for research, education and advocacy components of eHealth Initiative and Foundation (eHI). Convening senior executives from every group in healthcare to discuss, identify, and share best practices that transform the delivery of healthcare. Focus areas: improving health and wellness through innovative solutions; interoperability; privacy concerns; artificial intelligence; payment models to support innovative care; and tech tools for chronic care. She led development of dozens of national surveys and published groundbreaking reports. As part of her work with the Foundation, she led grants with California Health Care Foundation, Commonwealth Fund, Aetna Foundation and Bristol Meyers Squibb Foundation. Jennifer is co-chair of the Federal HIT Policy Committee’s Strategy and Innovation Workgroup; member of the HL7 Board of Directors; and a member of the Diabetes Collaborative Stakeholder Panel. Jennifer is a faculty member for the MHA and MHIA graduate programs at George Washington University. Prior to joining eHI, Jennifer headed up the strategic marketing at OpenNetworks, Inc., focusing on security solutions for the healthcare industry. She led healthcare industry relations at MicroStrategy, Inc., focusing on data-mining solutions for the pharmaceutical and healthcare industry. She spent four years at the National Committee for Quality Assurance as Director of Policy and Product Development, helping develop national quality standards for healthcare organizations. Jennifer began her career at the George Washington University Hospital, Medical Center and Health Plan working on quality management initiatives, clinical pathways and healthcare administration. Jennifer earned a master's in Human Resource Development, completed coursework in health administration doctoral program at GWU, and resides in Maryland with her husband and two children.
This webinar is supported by:

eHI Annual Meeting
eHI hosted its Annual Meeting from January 26-28th. Five panels discussed lessons learned, industry best practices, and how we move toward a more modern, technology-enabled, and equitable health care system. Panels of experts explored topics related to social determinants of health, health data privacy, policy and advocacy, and modern health care delivery.
For full biographies of panelists, click here.
Links to all videos below.
eHI CEO Jen Covich Bordenick Interviews Senator Catherine Cortez Masto (D-NV)
eHI was thrilled to host Senator Catherine Cortez Masto (D-NV) for a conversation on healthcare, data privacy, and the importance of federal policy to ensure transparency to the consumer.
Panel #1: TGI2021: Where Are We Heading This Year:
eHI CEO Jen Covich Bordenick was joined by outgoing Board Chair Dr. Susan Turney, President & CEO of Marshfield Clinic Health System, and incoming Board Chair Amy McDonough, Senior Vice President & General Manager of Fitbit Health Solutions. They discussed expectations for 2021, as well as wearable technology and a discussion on equality in healthcare providers.
"While attitudes have thankfully changed dramatically, we have not arrived at a fully equitable society."
- Dr. Susan Turney
Panel #2: Prioritizing Equality in COVID-19 Vaccine Distribution
eHI's Director of Strategy and Programs Wanneh Dixon joined Damika Barr, JD from Verily Life Sciences, Anna Basevich from Arcadia, J. Michael McGinnis, MD, MA, MPP from the National Academy of Medicine, and Diana Zuskov from LexisNexis Risk Solutions for a discussion on how to engage underserved communities in COVID-19 vaccine distribution and using data-driven approaches to close gaps in health equity.
"I think the biggest takeaway is that there is a lot of data out there and I think we're getting to the point where everyone is convinced data is important, but making it actionable and connecting it down to one individual that you can look at an entire data story for."
- Diana Zuskov
Panel #3: Virtual Care Delivery During COVID-19 and Beyond
eHI CEO Jen Covich Bordenick joined experts Saurabha Bhatnagar, MD of United Healthcare, Adam Pellegrini of CVS Health, and Roy Schoenberg, MD of Amwell. Panelists discussed how their organizations have scaled virtual care delivery during COVID-19 and how they envision the future of health care post-COVID-19.
"For the next generation of telehealth that we want to be known for it has to be built differently to allow for innovation of others to collaborate inside the telehealth encounters or surrounding the telehealth encounters."
- Dr. Roy Schoenberg
Panel #4: Protecting “Health-ish” Data: Balancing Innovation and Health Data Privacy
eHI's Vice President and Senior Counsel Alice Leiter joined Jodi Daniel, Partner at Crowell & Moring; Laura Hoffman, Assistant Direction of Federal Affairs at the AMA; and Liz Salmi, Senior Strategist, Research Communication at OpenNotes and Senior Multimedia Communications Director at Beth Israel Deaconess Medical Center. Panelists talked about the challenging balance of shoring up legal protections for the increasing amounts of non-HIPAA-covered health data, establishing consumer trust in new technologies, and encouraging innovation in health care and health tech.
"[With respect to the digital Covid contact tracing apps]... There was a great idea, a great need to try to supplement traditional contact tracing for public health purposes with the outbreak of Covid with digital apps and smartphone apps that could use different types of functionality on your phone ...to alert folks when they were exposed to Covid. Unfortunately, we saw with a lot of the early rollouts of those apps that people didn't trust what would happen to the information they provided."
- Laura Hoffman
Upcoming Webinar: Release of the Final Consumer Privacy Framework for Health Data. We are delighted to release our final proposal to shore up protections for non-HIPAA-covered health information and share our plans for phase 2 of our work. Please join us and our colleagues from the Center for Democracy and Technology on February 9 at 2:00.
Panel #5: Digital Health Policy: Have We Reached a Turning Point?
The last panel of the Annual Meeting was moderated by eHI’s Assistant Vice President of Policy, Catherine Pugh. Catherine was joined by Aashima Gupta, Director, Global Healthcare Strategy and Solutions at Google Cloud; Matthew Roman, Chief Digital Strategy Officer at Duke University Health System; and Dr. Mona Siddiqui, Senior Vice President, Clinical Strategy & Quality at Humana for a discussion on the impact of COVID-19 on health policy, lessons learned, and how we move forward to build a more effective, efficient, and equitable health care system.
“I think digital should have a level playing field and I think there’s often been just a much higher bar to get some things approved than in-person care, so my hope is that people begin to see last year as a proof point of what’s possible and continue to enable greater access to care for people through technology and through digital solutions.”
- Dr. Mona Siddiqui
WEBINAR: The Case for a Learning Health System: Lessons from COVID
When COVID-19 spread across the country, it took months for hospitals to piece together the best treatment options, share those learnings and for providers to adopt them. The traditional medical approach is too slow for today’s public health crises.
WEBINAR: New Strategies for Patient Engagement: Lessons Learned During the Pandemic
Are your patients and members so concerned about contracting COVID-19 that they are afraid to seek preventative care? Between deferred care, COVID-19 vaccine engagement, and the need to illuminate and address socioeconomic challenges and health equity, patient engagement presents new challenges as move into 2021. Do your current strategies measure up?
Please join us Lurie Children’s Pediatric Partners, an integrated network in Chicago, and Community Health Plan of Washington, a nonprofit health plan supporting Medicaid and Medicare populations, as they share their experiences and lessons learned from 2020, and discuss challenges ahead.
Both organizations knew early in the spring of 2020 that this year would make patient engagement difficult. They took this opportunity to rethink how they engaged with their populations by taking the lead in educating patients about the new public health threat, offering resources, and sharing guidance on preventative care.
The webinar will look at:
- Tools to support patients as the pandemic continues
- Engaging and educating patients around COVID-19 vaccinations
- Closing preventative care gaps and addressing deferred care
- Advancing health equity by addressing SDOH at the point of care
REGISTRATION NOTE: This webinar will be recorded and made available to registrants should the timing with Inauguration Day pose a conflict.
Speakers:

Anna Basevich
VP, Customer Success
Arcadia
Anna leads customer success at Arcadia, working with customers to build out tailored population health strategies that leverage Arcadia’s analytics and workflow tools. She oversees the execution of Arcadia’s strategic partnership programs, which expand the transformative impact of the Arcadia Analytics platform. Anna recently led the expansion of Arcadia’s customer training program to enable healthcare organizations to accelerate their value-based care outcomes.
Anna has worked with Arcadia customers – including health plans, ACOs, independent physician groups, IDNs, and life sciences organizations – across the country to develop and execute strategies to succeed in value-based care. She has deep experience supporting healthcare leaders as they implement effective enterprise-level programs to improve quality, manage cost and utilization, and drive accurate risk-adjusted payments. She leads and mentors Arcadia teams to help provider networks and health plan customers roll out Arcadia’s tools in an effective and targeted manner to end users and drive platform adoption and change management.
Anna has managed implementations and client services work at Arcadia and at Deloitte Consulting; her past work has included numerous programs around health system quality measurement and improvement under ACO and risk-based contracts, initiatives aimed at improving accuracy and completeness of documentation for risk adjustment, state health insurance exchange implementations, Patient Centered Medical Home transformations, Health Information Exchange strategy and analytics, and large-scale health IT implementations.
Anna received her Bachelor’s degree from Wellesley College.

Mackenzie M. Bisset, MSPH, MS, MBA
Director of Operations
Lurie Children’s Pediatric Partners
Mackenzie Bisset, MSPH, MS, MBA is currently the Director of Operations at Lurie Children’s Pediatric Partners where she oversees and manages the Clinically Integrated Network. She helps define the strategy of the CIN, and sets annuals goals; she hires and manages staff; manages vendor partnerships and subcontracts; implemented software to aggregate clinical data and maintain data feeds across the CIN; leads all marketing and communication efforts; and developed the CIN Quality and Safety Plan. She also helped negotiate and oversee the implementation of two Medicaid and three commercial VBCs totaling 140,000 lives and roughly $300 million in medical spend and has successfully achieved savings under these value-based arrangements.
Prior to directing the CIN, Ms. Bisset was the Clinical Quality Consultant for the Care Coordination Entity (CCE) at Lurie Children’s. As part of this role, she also identified opportunities for co-management between specialists and pediatricians; developed learning collaboratives to reduce costs; and improved the appropriateness of referrals while improving outcomes. Another component of her role was developing clinical care guidelines and quality and utilization metrics to ensure compliance with state requirements as well as identifying opportunities for performance improvement.
Additional previous titles include Accreditation Compliance/Health Services Accreditation Surveyor for the National Commission on Correctional Health care where she evaluated the health care services provided in jails and prisons across the United States. As a Consultant for Hubbert Systems Consulting, she provided subject matter advice on the structures and processes of health care delivery to clients, designed and implemented Quality Improvement and Patient Safety programs and more.

Jen Covich Bordenick
CEO
eHealth Initiative and Foundation
For over 20 years, Jennifer has focused on quality and innovative technology solutions to transform healthcare. As CEO, she provides leadership for research, education and advocacy components of eHealth Initiative and Foundation (eHI). Convening senior executives from every group in healthcare to discuss, identify, and share best practices that transform the delivery of healthcare. Focus areas: improving health and wellness through innovative solutions; interoperability; privacy concerns; artificial intelligence; payment models to support innovative care; and tech tools for chronic care. She led development of dozens of national surveys and published groundbreaking reports. As part of her work with the Foundation, she led grants with California Health Care Foundation, Commonwealth Fund, Aetna Foundation and Bristol Meyers Squibb Foundation. Jennifer is co-chair of the Federal HIT Policy Committee’s Strategy and Innovation Workgroup; member of the HL7 Board of Directors; and a member of the Diabetes Collaborative Stakeholder Panel. Jennifer is a faculty member for the MHA and MHIA graduate programs at George Washington University. Prior to joining eHI, Jennifer headed up the strategic marketing at OpenNetworks, Inc., focusing on security solutions for the healthcare industry. She led healthcare industry relations at MicroStrategy, Inc., focusing on data-mining solutions for the pharmaceutical and healthcare industry. She spent four years at the National Committee for Quality Assurance as Director of Policy and Product Development, helping develop national quality standards for healthcare organizations. Jennifer began her career at the George Washington University Hospital, Medical Center and Health Plan working on quality management initiatives, clinical pathways and healthcare administration. Jennifer earned a master's in Human Resource Development, completed coursework in health administration doctoral program at GWU, and resides in Maryland with her husband and two children.

Jennifer Polello, MHPA, PCMH CCE, MCHES
Senior Director of Quality and Population Health
Community Health Plan of Washington
Jennifer has over 20 years of extensive experience across the healthcare continuum in the areas of public health, chronic disease management, quality improvement, health policy, population health management and clinical informatics. She has exercised this experience from several points of view across the health care environment and has demonstrated expert facilitation skills in leading teams of clinicians, nurses and physicians through the transformation process of patient care in the ambulatory setting. Jennifer has worked on regional health information exchange projects and assisted in the design of a clinical decision support tool for patients with type 2 diabetes. She has also served as an Adjunct Clinical Assistant Professor mentoring PharmD candidates at Washington State University. Jennifer is currently leveraging her knowledge and expertise as the Senior Director of Quality and Population Health at Community Health Plan of Washington where she leads the company’s quality improvement strategies, population health and clinical data integration programs across the Network of 20 community health centers that operate more than 130 clinics across the state.
Support for this webinar brought to you by:

WEBINAR: The Next Wave: Automating Virtual Care
As the world adapts to the changes brought on in response to the coronavirus pandemic, it’s increasingly clear that virtual care is an essential component of modern care delivery. In response to the major pressures of care capacity and community safety, leading health organizations have adopted automated virtual care platforms to rapidly scale their care management capability. As we work to get the coronavirus pandemic under control, innovative leaders have also recognized the wide-ranging benefits of a richer, continuous and collaborative, care delivery process beyond addressing immediate needs brought on by the pandemic. The lasting impact delivered by virtual care at scale is coming into focus and helping inform how long term digital health initiatives benefit an organization in 2021 - and beyond.
In this topical session, we’ll explore a few ways in which market-leading healthcare provider organizations are leveraging the next wave of virtual care, how it informs their key long-term digital strategies and the positive outcomes that come with embracing automated virtual care at scale. Hear from national leaders in healthcare and technology as they discuss their journeys in expanding the use of automated virtual care to manage capacity challenges, deliver better patient experience, and improve population outcomes - all at a lower cost.
Speakers:
Jennifer Covich Bordenick
CEO, eHealth Initiative and Foundation
For over 20 years, Jennifer has focused on quality and innovative technology solutions to transform healthcare. As CEO, she provides leadership for research, education, and advocacy components of eHealth Initiative and Foundation (eHI). Convening senior executives from every group in healthcare to discuss, identify, and share best practices that transform the delivery of healthcare. Focus areas: improving health and wellness through innovative solutions; interoperability; privacy concerns; artificial intelligence; payment models to support innovative care; and tech tools for chronic care. She led development of dozens of national surveys and published groundbreaking reports. As part of her work with the Foundation, she led grants with California Health Care Foundation, Commonwealth Fund, Aetna Foundation and Bristol Meyers Squibb Foundation. Jennifer is co-chair of the Federal HIT Policy Committee’s Strategy and Innovation Workgroup; member of the HL7 Board of Directors; and a member of the Diabetes Collaborative Stakeholder Panel. Jennifer is a faculty member for the MHA and MHIA graduate programs at George Washington University. Prior to joining eHI, Jennifer headed up the strategic marketing at OpenNetworks, Inc., focusing on security solutions for the healthcare industry. She led healthcare industry relations at MicroStrategy, Inc., focusing on data-mining solutions for the pharmaceutical and healthcare industry. She spent four years at the National Committee for Quality Assurance as Director of Policy and Product Development, helping develop national quality standards for healthcare organizations. Jennifer began her career at the George Washington University Hospital, Medical Center and Health Plan working on quality management initiatives, clinical pathways and healthcare administration. Jennifer earned a master's in Human Resource Development, completed coursework in health administration doctoral program at GWU, and resides in Maryland with her husband and two children.

Murray Brozinsky
CEO
Conversa Health
Previously, Murray founded AVIH, an AI solution for primary care; co-founded and served as Chief Strategy Officer of Talix Inc. a risk adjustment SaaS company; and was Chief Strategy Officer of Healthline, a leading digital health education company for consumers, which he and the management team sold to Summit Partners in 2016. Prior to healthcare, Murray co-founded Loyalty Matrix (sold to Responsys/Oracle); Lypro Biosciences (sold to Cerenis Therapeutics); and Cambrian Technologies, his strategy and business development firm. Murray was President of Netcentives, a pioneer in digital loyalty and currency programs, which he helped take public. He started his career with stints at Boston Consulting Group and Morgan Stanley. Murray sits on the boards of First Call Ambulance Service and Adacado and is an advisor to Zignifica, Catelas, Aetho, UCSF Health Hub, and DeAnza High School Tech Academy.
Murray speaks and writes often about the future of healthcare. He recently gave keynotes at: Commonwealth Bank's Future of Health conference (2018 and 2017), Sydney; MUSC's Annual Healthcare Leadership Conference 2018, Charleston; The Healthcare Leaders Conference 2018, Dallas; Ogilvy’s HealthBot 2018 Summit, NYC; HealthXL’s Global Gathering 2018, London; the 2018 Academic Venturing Summit at JP Morgan, presented by Cleveland Clinic, San Francisco; and WBR Insights’ Healthcare 2020. He is interviewed frequently about digital health innovations, appearing in The New York Times, WSJ, Computerworld, Bankrate, Wired Magazine, and Health Innovation Media. Murray is also an award-winning playwright. His most recent play, Heavenly Bodies, won the 2017 Players Theatre Short Play Festival, NYC
Dr. Nick Patel
Chief Digital Officer, Prisma Health
Vice Chair for Innovation & Clinical Affairs, Dept. of Medicine, Adjunct Professor USC School of Engineering and Computing, Dept. of Integrated Computing
Practicing internist for the past sixteen years at Prisma Health, the largest, most comprehensive, non-profit hospital system in South Carolina. Currently serves as Chief Digital Officer at Prisma Health and Vice Chair for Innovation at USC Department of Medicine. Has given multiple presentations around the country on topics ranging from healthcare IT transformation, governance, workflow enhancements, health equity, telehealth, and population health. Subject matter expert for multiple Fortune 500 tech companies. Serves as a leader in defining and articulating a unique vision on the utilization and development of technology in healthcare. He currently serves on multiple Fortune 500 and University advisory boards. He also serves as Principal Investigator on multiple IRB approved IT studies in conjunction with USC and holds a clinical faculty position at the USC School of Medicine Department of Internal Medicine at USC School of Engineering and Computing. He is one of two physicians globally who have been awarded Microsoft's Most Valuable Professional Award and named Top 20 Chief Digital Officers to Know in 2020 by Becker's Hospital Review.

Dr. Aaron Neinstein
Associate Professor of Medicine, UCSF Endocrinology & Director of Clinical Informatics
UCSF Center for Digital Health Innovation
Aaron Neinstein, MD is Associate Professor of Medicine in the UCSF Divison of Endocrinology and Metabolism and Director of Clinical Informatics at the UCSF Center for Digital Health Innovation. He is board-certified in Internal Medicine, Endocrinology, and Clinical Informatics, with an active clinical practice focused on diabetes care. Dr. Neinstein, and inaugural inductee as a Fellow of the American Medical Informatics Association, has focused his career on empowering patients and physicians to better access, share, understand, and use health information for more connected collaborative care. He helped lead the Epic EHR implementation at UCSF and was on the founding team of Tidepool, a non-profit that creates open-source software to empower people with diabetes. At the UCSF CDHI, he leads a multi-disciplinary team focused on advancing interoperability and digital transformation of care delivery. Dr. Neinstein majored in American Studies at Northwestern University, graduated Alpha Omega Alpha from the Keck School of Medicine of USC, and did his Internal Medicine Residency and Endocrinology fellowship at UCSF.

Dr. Peter Pronovost, PhD
Chief Clinical Transformation Officer, University Hospitals
Dr. Peter Pronovost is a world-renowned patient safety champion, a practicing critical care physician, a prolific researcher, publishing over 800 peer-review publications, and a global thought leader, informing US and global health policy. His scientific work leveraging checklists to reduce catheter-related bloodstream infections has saved thousands of lives and earned him high-profile accolades, including being named one of the 100 most influential people in the world by Time Magazine, receiving a coveted MacArthur Foundation “genius grant” in 2008, and regularly recognized as one of the most influential executives and physician executives in healthcare. The life-saving intervention has been implemented state by state across the U.S. Today, these catheter infections that used to kill as many people as breast or prostate cancer, have been reduced by 80% compared to 1999 before the “To Err is Human” report was published. After demonstrating the ability to eliminate one harm in most health systems, Dr. Pronovost sought to eliminate all harms in one health system, Johns Hopkins. Toward that goal, Dr. Pronovost is the Johns Hopkins Medicine Senior Vice President for Patient Safety and Quality and the founder and director of the Johns Hopkins Medicine Armstrong Institute for Patient Safety and Quality. The Institute coordinates research, training, and operations for patient safety and quality across JHM, bringing together over 18 different disciplines from every school and division of the university. Drawing upon principles of high reliability, Dr. Pronovost created operating management system, integrating the governance, leadership, management, human resources, and data systems to improve safety and quality and to support learning and accountability. As a result, Johns Hopkins Medicine is significantly safer. Dr. Pronovost is working with several large health systems across the globe to implement this management system. Dr. Pronovost was elected to the National Academy of Medicine in 2011 and has received multiple honorary degrees. Dr. Pronovost is an advisor to the World Health Organizations’ World Alliance for Patient Safety and regularly addresses the U.S. Congress on patient safety issues. Dr. Pronovost regularly writes a column for the Wall Street Journal and US News and World Report. Dr. Pronovost is a founder of Doctella, a health information platform for quality of care. Dr. Pronvost serves as an advisor to HLM Venture Partners and as a senior advisor to Havencrest Healthcare Partners.
