Topic intro description here. Limited to 145 characters. Topic intro description here. Limited to 145 characters. Topic intro description here.
Provider Access to Patient Information Survey - 2017 Report
eHealth Initiative’s 2017 Provider Survey on Access to Patient Information examines perspectives on:
• Increased access to patient information
• Interoperability
• Changing regulations, including compliance with Merit-Based Incentive Payment System (MIPS) and Meaningful Use (MU)
• Latest findings on provider-related interoperability solutions, which drive outcomes and organizational priorities
After careful analysis of the survey results, the following key findings emerged:
- Key Finding 1: Patient engagement appears to be increasing, with more patients accessing their health information and managing how it is shared
- Key Finding 2: Providers are struggling to meet patient access regulations, which do not necessarily align with business needs
- Key Finding 3: Changing federal requirements, and the costs associated with them, are causing great concern among providers
- Key Finding 4: Current interoperability solutions do not meet the needs of providers
- Key Finding 5: Patient security, privacy and confidentiality remain top concerns amongst providers
- Key Finding 6: Professional societies and industry groups play a key role in educating providers on new regulations
- Key Finding 7: EHR vendors are viewed as “helpful” in addressing current patient access regulatory requirements
- Key Finding 8: Providers are engaged in a variety of alliances and participate in different interoperability frameworks
- Key Finding 9: Providers prioritize connectivity in a variety of ways
Webinar: Pulse on the Industry: Interoperability and Population Health Management
Please visit eHI's resource center for presentation slides, the webinar recording and a copy of the report.
The healthcare industry is moving the needle forward on interoperability and population health management. Our webinar, Pulse on the Industry: Interoperability and Population Health Management, examines the results of eHealth Initiative’s interview-based research project on the topic.
Consumer Mediated Exchange
Consumer Mediated Exchange, presented by Hon Pak, CMO, 3M Health Information Systems Division
Creating a Continuum of Seamless Care in Heart Health
Creating a Continuum of Seamless Care in Heart Health and a Culture of Collaboration
 On Tuesday, October 17, 2017, eHealth Initiative (eHI) hosted it’s second Continuum of Seamless Care Executive Meeting in Washington, DC. Twenty executive leaders, representing multiple industries and organizations, engaged in an enlightening discussion on the number one killer of all Americans, heart disease. This roundtable delved into the nuances faced by physicians and hospitals in their attempts to achieve seamless care, through reliable delivery of patient needs. The roundtable addressed improving patient outcomes, addressing fragmented care, and finding collaboration at the intersection of cardiology and radiology.
On Tuesday, October 17, 2017, eHealth Initiative (eHI) hosted it’s second Continuum of Seamless Care Executive Meeting in Washington, DC. Twenty executive leaders, representing multiple industries and organizations, engaged in an enlightening discussion on the number one killer of all Americans, heart disease. This roundtable delved into the nuances faced by physicians and hospitals in their attempts to achieve seamless care, through reliable delivery of patient needs. The roundtable addressed improving patient outcomes, addressing fragmented care, and finding collaboration at the intersection of cardiology and radiology.
Heart Disease in the U.S.
Laying the foundation for the day-long discussion was Chief of Cardiology at Montefiore-Einstein Medical Center in Bronx, NY, Dr. Ileana L. Piña. Her presentation, Heart Disease in America: Opportunities & Need for a Continuum of Care informed the group that heart disease is particularly detrimental to Black and Bible Belt communities in the U.S. and is already the number one cause of death globally [1]. Susan M. Campbell, Vice President of Public Policy at WomenHeart: The National Coalition for Women with Heart Disease, presented on the numerous disparities faced by women with heart disease. Participants noted that women are more likely to have heart attacks with no obstructive disease and that imaging works differently in women’s bodies [2].
For many years heart disease rates declined, for both men and women, thanks in part to concerted education and awareness efforts led by groups like the American Heart Association. Despite the fact that heart disease is effectively treatable with medication [3] [4] and reducing systolic blood pressure to 120 significantly reduces cardiovascular disease and mortality [5], deaths remain alarmingly high and are compounded by co-morbidities such as obesity. The number of hospitalizations for heart failure predict patient mortality. [6]
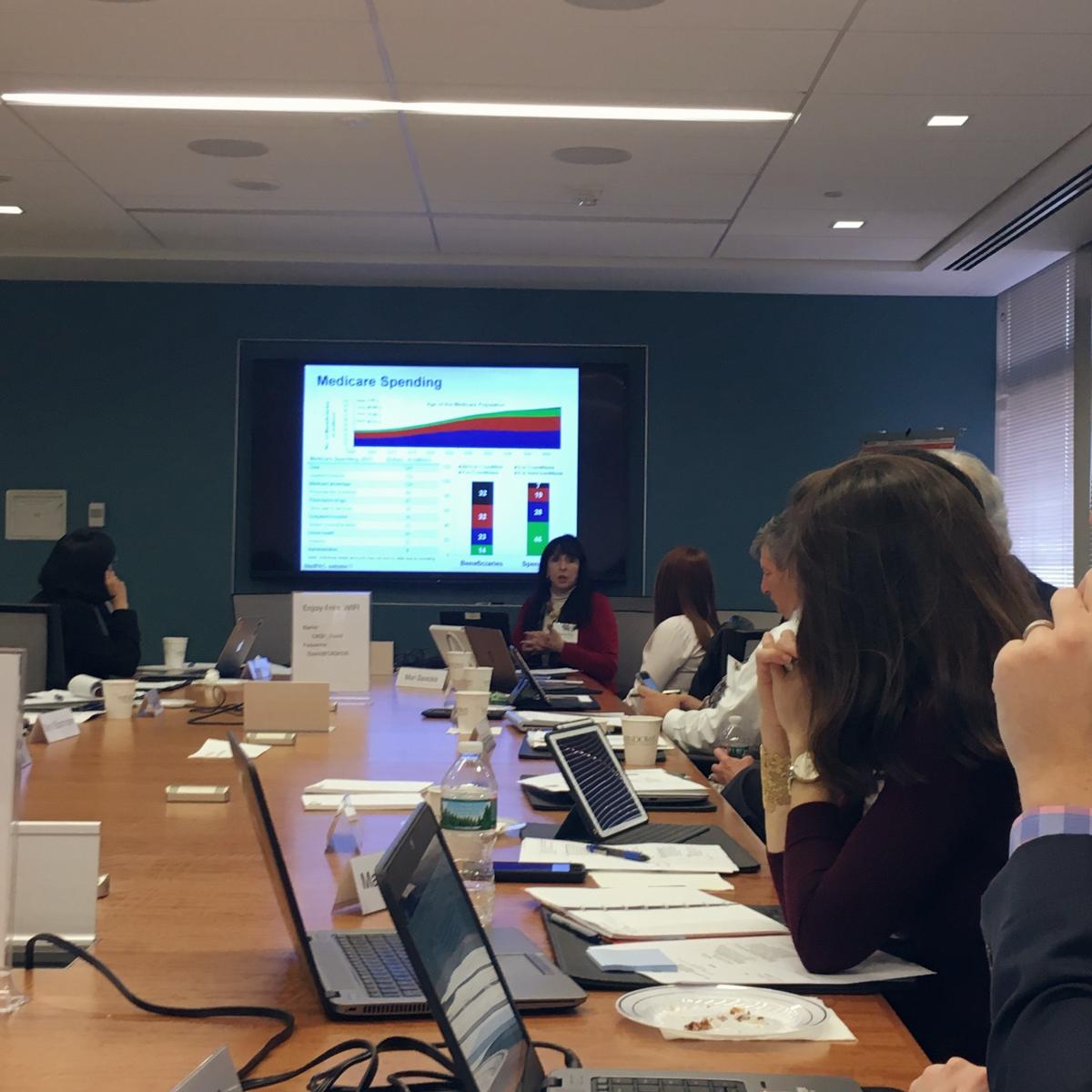 Dr. Piña’s presentation touched on many salient points about heart failure and its cost to healthcare:
Dr. Piña’s presentation touched on many salient points about heart failure and its cost to healthcare:
- If a hospital exceeds the 19.6% national readmission rate [7] within 30 days of initial discharge, the Centers for Medicare and Medicaid Services (CMS) withholds between 1-3% of reimbursements related to heart attacks, heart failure, and bypass surgery [8]
- Heart failure is the most common reason for patient rehospitalization within 30-days of discharge [9]
- Follow-up care within 7-10 days after hospital discharge is a CMS requirement and has proven to be beneficial for high risk patients [10], however 52% of patients receive no follow-up care within 30 days of discharge [11]
- More than 80% of patients who present in the Emergency Department (ED) with chronic heart failure are admitted to the hospital [12]
- Forecasts of the impact of heart failure in the US predict that costs will increase by more 120% between 2012 and 2030 [13]
|
“We are seeing an increase in mortality even though we are reducing hospitalization.” – Physician Participant |
Dr. Piña is leading an initiative to improve patient outcomes, which also creates financial savings for her institution. Process mapping was her key to success, as she learned the inner workings of various processes related to patient care. Making a follow-up appointment, at the time of discharge; conducting a comprehensive medicine reconciliation; and educating patients on when they needed to call the cardiologist were successful interventions that improved quality. After spending one-year training pharmacists on patient care related to cardiology, she initiated a “Brownbag Clinic” run by her hospital’s pharmacists. The Brownbag Clinic allowed patients to practice medication adherence and stop the use of unnecessary medication
Dr. Piña’s research mirrored key findings of eHealth Initiative’s September 19 eMAC Roundtable, a committee meeting on electronic medication adherence. The readmission rate for those participating in the Brownbag Clinic was 8% versus 24% in patients that did not participate.
 Telemedicine also played a role in improving outcomes for heart failure patients. The unequitable distribution of broadband across the U.S. was mentioned as an important factor in the implementation of telemedicine. Participant Meryl Blooomrosen, Senior Director of Federal Affairs at Premier reminded the group that coastal cities enjoy numerous broadband options, that are not available in parts of the country that are still reliant on DSL and dial-up connections. Broadband supports telehealth and virtual offices, which can only be a reality when communities have access.
Telemedicine also played a role in improving outcomes for heart failure patients. The unequitable distribution of broadband across the U.S. was mentioned as an important factor in the implementation of telemedicine. Participant Meryl Blooomrosen, Senior Director of Federal Affairs at Premier reminded the group that coastal cities enjoy numerous broadband options, that are not available in parts of the country that are still reliant on DSL and dial-up connections. Broadband supports telehealth and virtual offices, which can only be a reality when communities have access.
Radiology & Cardiology: Prevention, Diagnosis, New Technologies, and Seamless Care
Dr. Brian Choi, a cardiologist and professor at George Washington University led the discussion on radiology and cardiology’s role in prevention and diagnostics. Sharing their thoughts on achieving seamless care was Dr. William Borden, American College of Cardiology (ACC) Health Management Task Force member and George Washington University physician; and Dr. William Thorwarth, CEO of the American College of Radiology (ACR). The ACR and ACC have been developing Appropriate Use Criteria (AUC) for years, making a case for decision support tools and knowledge management systems that ensure evidenced based best practice data are routinely included in healthcare.
|
“It’s hard to put the patient first if territorialism drives decision making.” – Dr. Brian Choi |
Starting the conversation with tales from medical school, Dr. Choi illustrated how much territorialism is ingrained in medicine, often from the very beginning of medical training. Financial incentives can play a role in territorialism; however, it is further compounded by logistical barriers when data sharing is not feasible. There are some promising examples, as shared by participant Al Kinel, President of Strategic Interests. New York has a central repository for imaging reports, run by the local HIE. If institutions have IT systems that are configured for data sharing, the actual images can be also be shared. This example appears to be an anomaly.
Dr. Thorwarth shared his personal history of heart disease, reminding the group that radiologists are not immune to cardiological issues. In the age of value-based care, risk sharing by the patient has become an important component for healthcare. Patients are taking greater ownership of imaging and refusing the financial burden of repeating the same images with different practitioners. Providers are contemplating the best ways to get the most useful imaging data to the end user. For example, patients can purchase a portable EKG reader that attaches to their smart phone. The device takes medical-grade EKG readings and sends the results to their phone, which makes an appointment to check for abnormal heart rhythms or atrial fibrillation unnecessary.

Technology within radiology and cardiology is quickly advancing. The time-consuming process of reading every imaging report is now automated. Computers can read and indicate if an EKG study is normal, which allows practitioners to focus more closely on abnormal studies. Augmented or artificial intelligence (AI) is a promising development for risk stratification of imaging results. The consensus among roundtable participants was that AI will ultimately strengthen healthcare and will not replace radiologist. However, radiologist who are adept with AI will replace those who are not.
Along the vain of technology in cardiovascular health was information provided by Shawn Forrest, a Senior Lead Reviewer from the Cardiac Diagnostic Devices Branch of the U.S. Food and Drug Administration (FDA). There has been a substantial amount of changes in regulatory oversight over the last few years, increased transparency, and decreased time frames for device applications at the FDA. Guidance on clinical decision support should be published by the end of the year and will contribute to 21st Century Cures. The FDA continues to work on innovative projects such as addressing alarm fatigue in hospital Intensive Care Units (ICU) and streamlining the review of connective health functionality.
Key Takeaways
|
“We must fundamentally change the ways in which we deliver healthcare.” – Physician Participant |
- Doctors must reframe patient care, moving from episodes of care towards a collaborative, non-territorial continuum of care
- Fragmentation prevents information sharing among practitioners, however healthcare can move in the direction of seamless care with the push towards interoperability
- Process is always important
- Healthcare delivery must fundamentally change

References
- Cardiovascular diseases (CVDs), http://www.who.int/mediacentre/factsheets/fs317/en/
- Imaging Tests, Provocative Tests, Including Exercise Testing in Women with Suspected Coronary Artery Disease https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3433655/
- Advances In The Prevention And Treatment Of Cardiovascular Disease, http://content.healthaffairs.org/content/26/1/25.full.html&force=1
- Medications Used to Treat Heart Failure http://www.heart.org/HEARTORG/Conditions/HeartFailure/TreatmentOptionsForHeartFailure/Medications-Used-to-Treat-Heart-Failure_UCM_306342_Article.jsp
- Systolic Blood Pressure Reduction and Risk of Cardiovascular Disease and Mortality, https://jamanetwork.com/journals/jamacardiology/article-abstract/2629537?utm_source=Silverchair_Information_Systems&utm_campaign=FTM_05302017&utm_content=news_releases&cmp=1&utm_medium=email
- Repeated hospitalizations predict mortality in the community population with heart failure, https://www.ncbi.nlm.nih.gov/pubmed/17643574
- Rehospitalizations among patients in the Medicare fee-for-service program, https://www.ncbi.nlm.nih.gov/pubmed/19339721
- Hospital Readmissions Reduction Program, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4439931/
- Worse Prognosis in Heart Failure Patients with 30-Day Readmission, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5126448/#R05
- Transitional Care Management Services ICN 908628 December 2016, https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/Transitional-Care-Management-Services-Text-Only.pdf
- Timeliness of Outpatient Follow-up: An Evidence-Based Approach for Planning After Hospital Discharge, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4369604/#b5-0130115
- The Burden of Acute Heart Failure on U.S. Emergency Departments, http://www.sciencedirect.com/science/article/pii/S2213177914001024
- Forecasting the Impact of Heart Failure in the United States, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3908895/
Creating a Conduit for Better Health: Technology Connects Medical and Social Services
Kimber finally left when her husband tried to choke her and said he wished she was dead.
The marriage started out well, she tells her women’s shelter counselor, until he started drinking too much. Then the violence began. Today, she’s the mother of two young girls, without a job, a car, a home, personal security, family or social support.
Fortunately for Kimber, the shelter she found is part of Boulder County Department of Housing and Human Services’ integrated system of social services providers. She will only have to tell her story once, and the shelter worker will assess all her health needs—social, emotional, physical and financial. She’ll help Kimber sign up for Medicaid coverage for the family, apply for food and housing assistance, job training, mental health counseling, transportation and shelter. In Boulder County, they call this a no-wrongdoor approach to serving clients.
What’s more, Kimber’s assessment data will be entered, real-time, into an integrated data warehouse. Dozens of organizations— serving social, mental and physical health needs—will be able to find her in this system. They can add notes to the record as services are provided, or as case managers create a care plan—with Kimber—to help her achieve her goals. And Kimber can also access her information through a client portal—so she can track her own progress.
Connecting health care providers through an electronic records platform is not a new concept; about 99 percent of U.S. hospitals had partially or completely implemented electronic health records in 2016, with many allowing at least limited access by contracted physician offices and group practices.1 Less pervasive, but not uncommon, are health information exchanges (HIEs) that allow health care providers and patients to access and securely share a patient’s medical information electronically.
An S-HIE brings together the many community-based organizations that meet client needs for the social determinants of health—such as housing, food, safety, transportation and employment—and links them with organizations that provide mental, behavioral and physical health services as well. It’s a bridge connecting health care delivery and the real-life circumstances in which people live, work and play—the social determinants of health that contribute to our nation’s high health costs.
Connecting Communities Collaborative: The Critical Role of HIEs in Disaster Response
Presentation slides and recording for 10/26/17 Connecting Communities Collaborative
Connecting Communities Collaborative inaugural meeting on Thursday, October 26 -- a retrospective of the important role HIEs have played during Hurricanes, from Katrina to Harvey.
When Hurricane Katrina reached Louisiana in 2005, the number of physicians using electronic medical records was minimal. The concept of health information exchanges were mostly a conversation on the future of healthcare. Evacuees fled Louisiana, settling in Texas, and other states, without medical records, medication histories, or prescriptions. Paper records were destroyed and the need for HIEs was much more evident. Now in 2017, the landscape has changed dramatically, with HIEs creating a different world for those affected by Hurricane Harvey.
Discussion led by Doug Dietzman, Executive Director of Great Lakes Health Connect. Other panelists include:
- Phil Beckett, PhD, Chief Technology Expansion Officer, HASA Health Information Exchange
- Nick Bonvino, CEO, Greater Houston HealthConnect
Creating a Continuum of Seamless Care, Heart Health
Presentation slides from 10/17/17 Executive Roundtable on Creating a Continuum of Seamless Care in Heart Health. By William T. Thorwarth Jr. MD, FACR, CEO of the American College of Radiology.
Heart Disease in America: Opportunities & Need for a Continuum of Care, Focus on Heart Health
Presentation slides from 10/17/17 Executive Roundtable on Creating a Continuum of Seamless Care in Heart Health. By Ileana Pina, MD, MPH.
Rehospitalizations among Patients in the Medicare Fee-for-Service Program
Aricle from Jencks and Coleman (2009) in the New England Journal of Medicine analyzing Medicare claims data from 2003-2003 to describe the patterns of rehospitalization and the relation of rehospitalization to demographic characteristics of the patients and to characteristics of the hospitals.
CADS-RADS Coronary Artery Disease - Reporting and Data
An expert consensus document of the Society of Cardiovascular Computed Tomography (SCCT), the American College of Radiology (ACR) and the North American Society for Cardiovascular Imaging (NASCI). Endorsed by the American COllege of Cardiology. The intent of CAD-RADS e Coronary Artery Disease Reporting and Data System is to create a standardized method to communicate findings of coronary CT angiography (coronary CTA) in order to facilitate decision-making regarding further patient management. Cury et al. (2016)
