Webinar: Avoid Unintended Bias: How to Responsibly Use AI/Machine Learning to Address Health Disparities
A Thought Leadership Series with UnitedHealth Group
Activity Description
Artificial intelligence (AI) and machine learning (ML) are increasingly being used in healthcare settings with applications in decision support, patient care, and disease management. If the underlying data on which AI depends is inherently biased or lacks a diverse representation of populations, the algorithms cannot produce accurate outputs and will further widen the gap of equitable care.
This activity will discussed how AI and ML can be used to address social determinants of health and create more equitable healthcare solutions and improve health outcomes.
Learning Objectives
- Identify approaches to create inclusive data sets that produce positive health outcomes for all patients.
- Recognize processes that can result in biased data.
- Illustrate how providers can properly use innovative technology, like AI and ML, without compromising patient safety and experience.
- Distinguish collaborations necessary to ensure that future AI and ML technology will optimally integrate and produce accurate data that can improve health outcomes, and how to initiate collaboration within the organization.
Speakers
- Moderator: Michael Currie, Chief Health Equity Officer, UnitedHealth Group
- William Gordon, MD, Senior Advisor - Data and Technology, Center for Medicare and Medicaid Innovation
- Kevin Larsen, MD, FACP, Senior VP, Clinical Innovation, Optum
- Elia Lima-Walton, MD, Director Data Science and Clinical Analytics, Elsevier
Sponsored By:

EHI and LexisNexis® Risk Solutions Release Report on Incorporating SDoH Into Community Health Programs
Washington, DC – March 16, 2023 – Today, Executives for Health Innovation (EHI) and LexisNexis® Risk Solutions released the report, Incorporating SDoH Into Community Health Programs. This report provides an expert overview of the important elements of incorporating social determinants of health (SDoH) into a Community Health Program (CHP) strategy – to provide interventions for vulnerable populations.
Report: Incorporating SDoH Into Community Health Programs
Overview
|
Over the last decade, researchers have identified how social determinants of health (SDoH) impact vulnerable communities. Social determinants of health (SDoH) are the nonmedical factors that influence health outcomes. It’s generally agreed that SDoH factors can be broken into five categories: education access, quality healthcare, strong neighborhood and built-environment, economic stability, and social and community context. SDoH data provides an additional layer of valuable information to help clinicians and public health experts better understand their populations. Community Health Programs (CHPs) are continuing to incorporate elements of SDoH into their work serving patients. Recently, Executives for Health Innovation (EHI) spoke with experts in SDoH and Community Health Programs to explore the use of SDoH in CHPs. This paper provides an overview of the important elements of incorporating SDoH into a community health strategy. EHI thanks LexisNexis® Risk Solutions for their generous support of this report and their continued support of our organization’s work in realizing a society where everyone has a fair and just opportunity to be as healthy as possible.
|
|
Webinar: Closing the Gap of Care Inequality for Vulnerable Individuals and Their Communities
A Thought Leadership Series with UnitedHealth Group
Activity Description
Achieving health equity, eliminating disparities, and improving health for all is the ideal goal within an organization. Closing the gaps to improve quality of life, health, and overall well-being regardless of one's socioeconomic, cultural, or educational status, or the level of other social determinants of health is essential in establishing a solid program foundation. This activity discussed how organizations must build health equity programs into their core business structure and develop strategies that are relevant, actionable, measurable, and based on the latest data - and the significance of an organizational strategy to close the healthy equity gap.
Learning Objectives
- Illustrate how to start a conversation with leadership about approaches to improve health equity within their organization.
- Identify factors that influence the development of a sustainable health equity strategy within an organization.
- Determine strategies to measure a health equity program’s maturity and ability to ensure lasting positive outcomes.
- Assess the steps of health equity program development that are essential to establish a solid program foundation.
Featured Speakers
- Moderator: Kevin Larsen, Senior VP, Clinical Innovation, Optum
- Joseph Betancourt, MD, MPH, President, The Commonwealth Fund
- Michael Currie, Chief Health Equity Officer, UnitedHealth Group
- Lauren Smith, MD, MPH, Chief Health Equity and Strategy Officer, CDC Foundation
Sponsored By:

Blog: Health Equity – It’s Time for Bold Thinking and a Focus Shift to the Upstream Drivers
Yele Aluko MD, MBA, FACC
It is instructive that in 2002, the US Congress commissioned the National Academy of Sciences to determine the extent and drivers of racial and ethnic disparities in US healthcare. Subsequently, twenty years ago in 2003, the “Unequal treatment” report was published by the Institute of Medicine (IOM)1. Through the review of more than 300 peer reviewed scientific studies and papers, it validated unequivocally that racial and ethnic disparities in healthcare do exist, departing from the hitherto presumed understanding that genetic predispositions to disease in racial minorities were the driving factors. Indeed, it was established that many factors within health systems and US society including systemic racism were and continue to be driving contributors. The year 2003 was indeed the first time in US history that scientific acknowledgment and public awareness of racism as a driver of health disparities in US medicine was established.
This observation of societal inequity is not unique to healthcare. The reality that racial inequality permeates every facet of American society can no longer be disputed. But it is critical to understand that the relics of the historic political drivers in US history explain much of what we see today in mainstream society manifesting as racial disparities in education, criminal justice, housing, economic stability, and more specifically in the health industry2. Furthermore, it is now better understood that these health disparities are pervasive within the broader portfolio of vulnerable populations including gender, the elderly, children, immigrants, LGBTQ persons, the homeless and all who are disenfranchised, race irrespective3.
The annual economic burden4 of health disparities is profound and projected to be in excess of $230B by 2050 if current trajectories continue. The opportunity cost is projected to be up to a $5T loss to the US economy over the next 5 years if racial gaps for just black Americans are not closed by then. These numbers do not account for the broader population of people vulnerable to health inequities.
The business value derived by achieving health equity is compelling – with one estimate suggesting that eliminating health disparities would yield $135B in annual economic gains5. Still yet, many organizations struggle with how to not only apply but also justify health equity principles within their business. If it is presumed that majority of Americans are aligned on the moral imperative to achieve health equity (HEQ), it is becoming increasingly clear that we need to understand both the qualitative (perceived improvement in patient experience and quality of care), and quantitative value (cost reduction, margin relief, increased revenue and market share growth) to be derived from HEQ, and by so doing provide the business with objective insight into how to approach HEQ transformation with proactive intelligence and a potential ROI.
So why now, twenty years after the IOM report is there such renewed vigor and a call for increased rigor around the health equity conversation? The COVID experience shed light on the pervasive degree of these health disparities in the US, and more so on the failure of the health industry to prioritize correction. This has now led to a trifecta of legislative focus, regulatory surveillance and a growing awareness of the ignored market opportunity that is catalyzing the transition from viewing health equity through an academic lens, and as a social and moral obligation only, moving the conversation to a strategic priority within C-suites in the healthcare sector, corporate America and in the White House6.
Concurrently, the Center for Medicare and Medicaid Services7 and The Joint Commission for Accreditation of Healthcare Organizations8 have developed specific metrics by which health systems will be measured and held accountable for developing and executing on health equity delivery. These regulatory requirements are expected to incentivize health organizations to invest in health equity and to extend resources to understand the business case for so doing. With these understandings, and with the emergence of meaningful commitments to drive health equity, there are critical questions that we must now ask and answer to succeed, objectively, transparently and honestly.
We must now ask;
- Why have prior health equity efforts failed to drive systemic impact?
- What can we learn from these failed efforts to ensure accountability for success going forward?
- Are we aligned on the need to shift the focus away from just downstream interventions to the root cause of these inequities – the political determinants of health undergirded and driven by systemic racism that manifest by default in health inequities in US medicine?
- Are we ready to be bold enough to engage in uncomfortable conversations on inequities stemming from race, ethnicity, place, and class?
The time is now for all well-meaning stakeholders in the health equity ecosystem to move beyond the social and moral obligation of society as the only levers to address heath inequity. They must now embrace the compelling business case to do so, but most importantly they must align on the reality that the focus must shift to accepting the impact of structural racism as a primary lever that must be remediated to be successful in driving impact towards health equity delivery.
[1] Unequal treatment: report of the Institute of Medicine on racial and ethnic disparities in healthcare - PubMed (nih.gov)
[2] Annie E. Casey Foundation's Kids Count Data Center
[3] Vulnerable Populations: Who Are They? (ajmc.com)
[3] https://altarum.org/sites/default/files/uploaded-publication-files/WKKellogg_Business-Case-Racial-Equity_National-Report_2018.pdf
[4] THE BUSINESS CASE FOR RACIAL EQUITY,” W.K. Kellogg Foundation website
[5] Advancing Equity and Racial Justice Through the Federal Government | The White House
[6] CMS Framework for Health Equity | CMS
[7] Make Health Care Equity a Leader-Driven Priority | The Joint Commission
About the Author
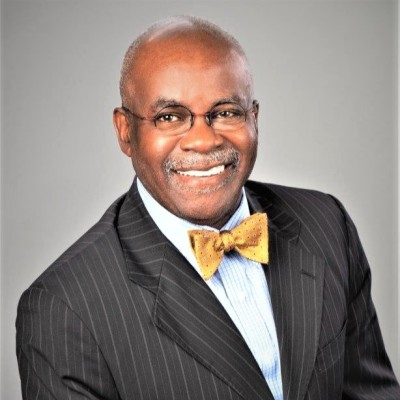
Yele Aluko MD, MBA, FACC
Dr. Aluko is a board-certified interventional cardiologist, chief medical officer at EY, and director of the EY Center for Health Equity. He is a member of the EHI Board of Advisors.
These views expressed by the author are not necessarily those of Ernst & Young LLP or other members of the global EY organization.
Webinar: Avoid Unintended Bias: How to Responsibly Use AI/Machine Learning to Address Health Disparities
This activity will discuss how AI and ML can be used to address social determinants of health and create more equitable healthcare solutions and improve health outcomes.
Webinar: Closing the Gap of Care Inequality for Vulnerable Individuals and Their Communities
This activity will discuss how organizations must build health equity programs into their core business structure and develop strategies that are relevant, actionable, measurable, and based on the latest data - and the significance of an organizational strategy to close the healthy equity gap.
EHI and Philips Release Report on Inequity in Cancer Care
Washington, DC – December 13, 2022 - Today, Executives for Health Innovation (EHI) and Philips released the report, Addressing Inequity in Cancer Care.
Report: Addressing Inequity in Cancer Care
Overview
Inequities in cancer research and care are widespread. As more clinical data is analyzed and collected, the gaps in care for vulnerable communities have only become more glaring. A 2022 BMC Public Health study found that cancer survival rates were lower for individuals living in both a high-income country and a resource-deprived community (BMC Public Health 2022). Statistics and studies like this are bolstering research initiatives across the country.
In a recent, multi-stakeholder roundtable, Executives for Health Innovation (EHI) convened leading experts to address the widening gaps that exist in oncology care and screening for those in vulnerable populations. The attendees addressed the need for collaboration between public and private industries (including Moonshot 2.0) to make meaningful changes and improvements.
A summary of the key concerns and highlights from the discussion are offered in this report.
With generous support from Philips

Policy Briefing: The Government’s Role in the Future of Ethical Digital Health Innovation
Overview
Dr. John Halamka, President of Mayo Clinic Platform, discusses the importance of public/private partnerships inside the healthcare technology ecosystem. He explains how the government can foster, and not stifle, the innovative tools being created to enhance patient care and ensure positive health outcomes through necessary guidelines, guardrails, and the push for transparency of data collection, protection, and clean data-set composition.
Dr. Halamka explains why there is a need to set a standard metrics with which researchers can use to measure the performance of their AI models in healthcare.
Featured Speaker
- John Halamka, M.D., M.S., President, Mayo Clinic Platform






