Prior Authorization: Current State, Challenges, and Potential Solutions
 The prior authorization (PA) process is entrenched in today’s healthcare system. Prior authorization is a decision by a payer that a healthcare service, treatment plan, prescription drug, or durable medical equipment is medically necessary and is included in a member’s coverage. Although PA is meant to ensure appropriate, cost-effective healthcare, it often creates barriers and administrative burdens for providers, payers, and patients. In a world where rovers roam capably on Mars, PA is still a broken process. Fixing PA will alleviate stress for patients and providers and reduce costs for healthcare as a whole.
The prior authorization (PA) process is entrenched in today’s healthcare system. Prior authorization is a decision by a payer that a healthcare service, treatment plan, prescription drug, or durable medical equipment is medically necessary and is included in a member’s coverage. Although PA is meant to ensure appropriate, cost-effective healthcare, it often creates barriers and administrative burdens for providers, payers, and patients. In a world where rovers roam capably on Mars, PA is still a broken process. Fixing PA will alleviate stress for patients and providers and reduce costs for healthcare as a whole.
In Fall 2018, eHealth Initiative (eHI) and Virence Health (now a part of athenahealth) embarked on a project to find practical solutions for fixing PA. eHI began the endeavor by gathering feedback from high-level executives during structured interviews, specifically:
- Provider perspectives on PA and appropriate use criteria in the workflow
- Organizational approaches to implementing PA
- Strategic organizational goals around PA
- Barriers limiting the automation and implementation of PA
- Actions that policymakers, payers, and patients could take to improve PA
These interviews set the groundwork for two roundtable discussions that convened multiple stakeholders throughout healthcare. Stakeholders were well versed in the subject of PA, representing the issue from various perspectives with hundreds of years of collective experience in the health IT sector. As a component in eHI’s Prior Authorization Initiative, this brief discusses the current state of PA, and offers examples of initiatives, from the field, that are working to address PA. Download the full report below.
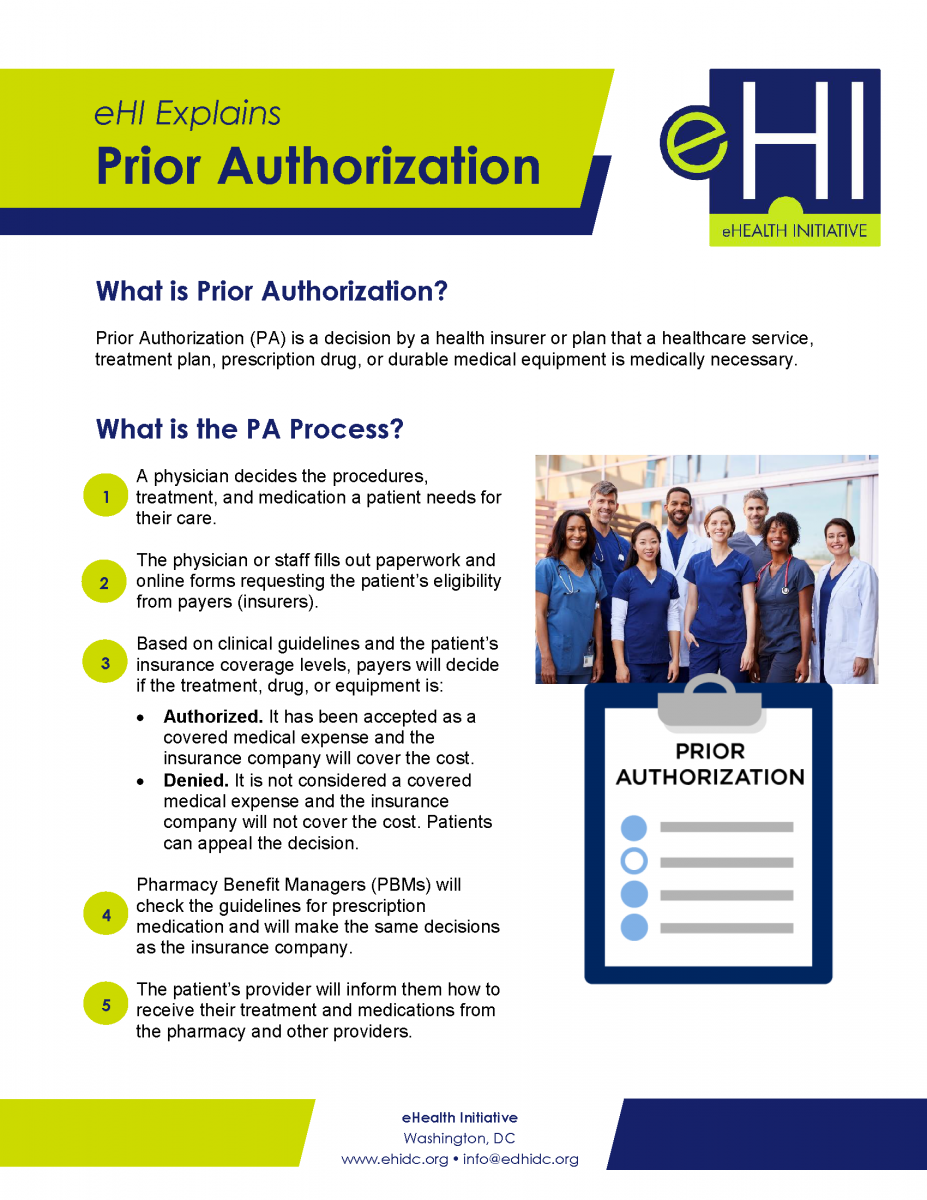
eHI Explains Prior Authorization
Prior Authorization is a decision by a health insurer or plan that a healthcare service, treatment plan, prescription drug, or durable medical equipment is medically necessary. This document gives a simple explanation of the Prior Authorization process and provides an overview of eHealth Initiative's Prior Authorization Project and considerations for improving Prior Authorization. Download the document below.
Considerations for Improving Prior Authorization Document
 In 2018 and 2019, eHealth Initiative (eHI) convened a series of prior authorization workshops with representatives from key stakeholder organizations across healthcare. The goal of the workshops was to establish a set of recommended practices to help improve the current prior authorization environment and to respond to the widespread challenges and dissatisfaction healthcare professionals have with prior authorization.
In 2018 and 2019, eHealth Initiative (eHI) convened a series of prior authorization workshops with representatives from key stakeholder organizations across healthcare. The goal of the workshops was to establish a set of recommended practices to help improve the current prior authorization environment and to respond to the widespread challenges and dissatisfaction healthcare professionals have with prior authorization.
United States healthcare spending grew to $3.5 trillion by the end of 2017, and approximately 1 in 3 dollars of those expenditures do not actually improve health. Experts estimate that about 30% of health spending is wasted on unnecessary services, excessive administrative costs, fraud, and other problems. Prior authorization is also meant to optimize patient outcomes and protect their safety. Healthcare payers utilize prior authorization to keep costs in check while reducing waste; error; and unnecessary procedures, treatments, and prescriptions.
The prior authorization process has, however, proved burdensome for healthcare professionals (clinicians, nurses, physicians, and others who provide care directly to patients) and can result in delayed or denied patient care. A recent American Medical Association (AMA) survey revealed that 86% of physician respondents feel that the burden associated with prior authorization in their office is either “high or extremely high” and that they and their staff spend an average of 14.9 hours each week to complete the prior authorization workload.
Download the full report below.
.
Cigna Eclipses 50% In Value-Based Care Pay To Providers
Cigna Eclipses 50% In Value-Based Care Pay To Providers
Cigna says it’s paying more than half of its reimbursements to medical care providers in its top markets via value-based models that are quickly overtaking fee-for-service medicine in the U.S.
Value-based pay is tied to health outcomes, performance and quality of care of medical-care providers who contract with insurers via alternative payment vehicles like accountable care organizations (ACOs), a delivery system that rewards doctors and hospitals for working together to improve quality and rein in costs.
The full Forbes article can be viewed at this link.
Empathy: A critical ally in battling physician burnout
Empathy: A critical ally in battling physician burnout
With almost half of doctors nationally experiencing burnout, one medical group turned to physician empathy training. Learn how empathy reduces burnout.
At the Northeast’s largest nonprofit independent medical group, 48 percent of physicians reported burnout. That high rate of physician burnout—fed by the competing demands of contemporary medical practice—can make cultivating a healthy sense of empathy a struggle. That, in turn, can negatively affect professional satisfaction, which is why this medical group’s journey to reducing burnout began with physician empathy training.
While physicians are commonly viewed as being empathetic, their behavior might come across differently to the patient in the room. The physician might seem rushed, distracted or trying to squeeze too much into one visit while simultaneously entering notes on the computer, said Steven Strongwater, MD, president and CEO of Atrius Health. The Boston-area medical group’s 1,300 clinicians deliver care to more than 720,000 patients.
Committed to making physician burnout a thing of the past, the AMA has studied, and is currently addressing issues causing and fueling physician burnout—including time constraints, technology and regulations—to better understand the challenges physicians face.
The full American Medical Association article can be viewed at this link.
2019 HEALTHCARE TRENDS FORECAST: THE BEGINNING OF A CONSUMER-DRIVEN REFORMATION
2019 HEALTHCARE TRENDS FORECAST: THE BEGINNING OF A CONSUMER-DRIVEN REFORMATION
The well-known proverb “may you live in interesting times” is considered by many to be a blessing, yet others believe it is actually an ancient curse. People’s interpretation tends to correspond with their own appetite for change, as well as their comfort (or lack of) in the face of ambiguity. Regardless of the adage’s origin and intent, many would agree that these are interesting times for healthcare. In fact, at HIMSS we believe healthcare is currently undergoing a period of reformation on a scope and scale that is unmatched.
A perfect storm of factors – including the shift toward value-based care, rising costs, health system consolidation, the approaching silver tsunami, regulatory pressures, increased consumerization, major technology players entering the market and the ever-expanding potential of digital health tools – are coalescing and fundamentally disrupting business models. Traditional healthcare institutions are in reactive mode. Upstarts are finding that healthcare is not as easily disrupted as industries like retail. For nearly everyone, there are more questions than answers.
At HIMSS, we believe it is our responsibility to help the industry make sense of these changes and tap into the promise and potential of information and technology. With that premise, we are introducing an annual forecast report. Bringing together insights from leadership across HIMSS and our subsidiaries, we’re aiming to shine a light around the corner and help illuminate the path to clinical and financial health.
Read on for our predictions for the industry in 2019.
The full article can be downloaded below.
Can Digital Medicine Improve Drug Adherence?
Can Digital Medicine Improve Drug Adherence?
Lack of proper adherence to medications has been called a national epidemic. To help address the adherence problem multiple digital health solutions have been proposed with some concerns that there has been limited large-scale evidence to support adoption. A new program focused on oncology patients is attempting to make a difference using a value-based payment structure between a health system and technology company.
The full Forbes article can be viewed at this link.
The Deadly Consequences Of Financial Incentives In Healthcare
The Deadly Consequences Of Financial Incentives In Healthcare
For decades, elite business schools have touted the benefits of financial incentives to motivate sales teams, factory workers and rising executives. Results are mixed.
In medicine, financial incentives rarely achieve their intended goals. It’s not because they don’t work. As I tell students at the Stanford Graduate School of Business, it’s because they work too well.
Monetary rewards always change doctor behavior, but rarely achieve the outcomes desired—something my predecessor learned the hard way when he tried to increase patient satisfaction.
This article also provides alternative best practices for improving patient satisfaction that avoids many of the discussed pitfalls of financial incentives.
Best Practices
- Transparency - Unblind the patient-satisfaction data for every physician and make the figures available for all to see. This allowed everyone to assess their own strengths and weaknesses.
- Education - We created educational programs to help physicians improve their satisfaction scores with personal coaching and development opportunities.
- Convenient access to care - We made it easier for doctors to satisfy patients by offering convenient access to care through technology.
The full Forbes article can be viewed at this link.
What would happen if hospitals openly shared their prices?
What would happen if hospitals openly shared their prices?
Hospitals have resisted disclosing prices, leading policymakers to consider laws requiring price transparency. This issue has taken on increasing urgency, as patients face increasing out-of-pocket costs. In addition, prices vary widely across hospitals. The same lower limb MRI can cost US$700 at one hospital and $2,100 at another. This means that there are large potential savings if patients switched to less expensive options.
There was a tiny step in this direction on Jan. 1, when all hospitals in the U.S. were required to post their charge prices. However, the list of over 15,000 procedures is notoriously incomprehensible, even for medical professionals. What exactly is a “HC PTC CLOS PAT DUCT ART,” a procedure listed by one Tennessee hospital? Perhaps more importantly, patients’ out-of-pocket costs often depend on the specifics of their insurance plan and the prices that are negotiated by their insurer, meaning the listed prices do not reflect what they actually pay.
For these reasons, many researchers and commentators, including myself, believe that this approach is unlikely to have a meaningful effect on health care costs.
That does not mean that price transparency is hopeless. Recent research shows that price transparency tools that actually have useful, easy-to-use information can benefit patients and reduce health care costs.
The full The Conversation article can be viewed at this link.
Assessing the Unintended Consequences of Health Policy on Rural Populations and Places
Assessing the Unintended Consequences of Health Policy on Rural Populations and Places
Because of the complexity of the U.S. health care system, thoughtfully designed health policies carry a risk of having unintended consequences, particularly for health systems in rural places that have place-based fundamentals that deviate substantially from urban and suburban areas. Policies developed without consideration of rural contexts are likely to create unanticipated and negative consequences for rural residents, providers, and communities.
When health policies are being developed, a number of themes that emerge are useful to keep in mind. Specifically, how will this policy impact the ability of a rural health system to offer essential, affordable, and high-quality services to rural populations? How might this policy result in disparate outcomes and widen health inequities, such as threatening access, slowing quality improvement, or creating financial barriers to obtaining health insurance or buying health care services?
The rural-proofing framework presented in this paper is a policy analysis tool for thinking about what the unintended consequences of a policy may be on rural populations and places vis-à-vis the objectives of a high-performance rural health system. Policy analysis must be applied to all sources of authoritative actions given that policies are produced not just in the legislative context, but also through judicial, administrative, and rulemaking actions.
The full report can be downloaded below.