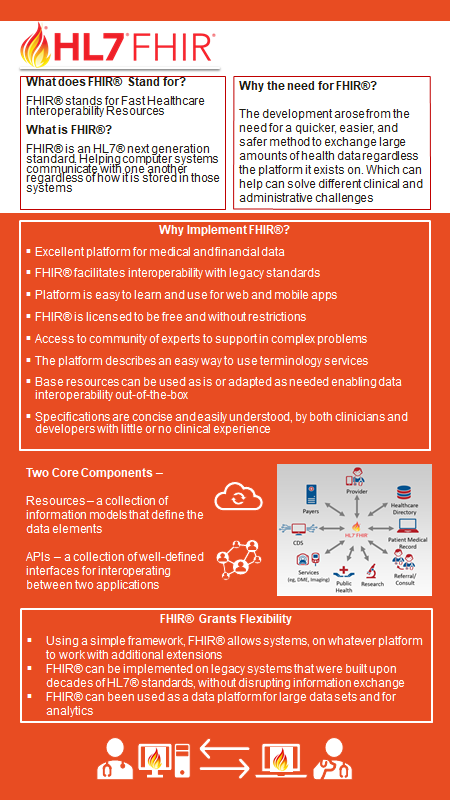
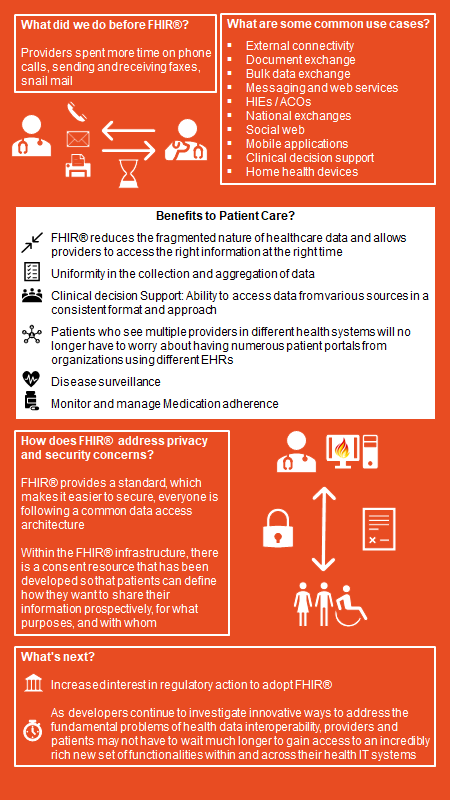
FHIR FAQs
The following is a FAQ document that explains what FHIR is and some of the potential benefits of wide-spread adoption.
Barriers to Use of Telepsychiatry: Clinicians as Gatekeepers
Telepsychiatry is effective and has generated hope and promise for improved access and enhanced quality of care with reasonable cost containment. Clinicians and organizations are informed about clinical, technological, and administrative telepsychiatric barriers via guidelines, but there are many practical patient and clinician factors that have slowed implementation and undermined sustainability. Literature describing barriers to use of telepsychiatry was reviewed.
PubMed search terms with date limits from January 1, 1959, to April 25, 2019, included telepsychiatry, telemedicine, telemental health, videoconferencing, video-based, Internet, synchronous, real-time, two-way, limitations, restrictions, barriers, obstacles, challenges, issues, implementation, utilization, adoption, perspectives, perceptions, attitudes, beliefs, willingness, acceptability, feasibility, culture/cultural, outcomes, satisfaction, quality, effectiveness, and efficacy.
Articles were selected for inclusion on the basis of relevance. Barriers are described from both patient and clinicians' perspectives. Patients and clinicians are largely satisfied with telepsychiatry, but concerns about establishing rapport, privacy, safety, and technology limitations have slowed acceptance of telepsychiatry. Clinicians are also concerned about reimbursement/financial, legal/regulatory, licensure/credentialing, and education/learning issues. These issues point to system and policy concerns, which, in combination with other administrative concerns, raise questions about system design/workflow, efficiency of clinical care, and changing organizational culture. Although telepsychiatry service is convenient for patients, the many barriers from clinicians’ perspectives are concerning, because they serve as gatekeepers for implementation and sustainability of telepsychiatry services. This suggests that solutions to overcome barriers must start by addressing the concerns of clinicians and enhancing clinical workflow.
Read more by clicking the link below.
Older Clinicians and the Surge in Novel Coronavirus Disease 2019 (COVID-19)
The recent report of critically ill emergency physicians infected by the novel coronavirus disease 2019 (COVID-19) is a sobering reminder of the vulnerability of the nation’s health care workforce. While all members of the health care workforce are vital as the health care system faces perhaps its greatest challenge in memory, physicians and nurses are the caregivers who typically have the most direct contact with patients, whether through advising, triaging, or treating those who require hospitalization. Hospitals and other care delivery organizations, including state and local health departments, should carefully consider how best to protect and preserve their workforce, with careful consideration involving older physicians and nurses.
Read more of this viewpoint by clicking this link below.
Anywhere to Anywhere: Use of Telehealth to Increase Health Care Access for Older, Rural Veterans
Rural veterans are older and have more complex medical issues than their urban counterparts. Veterans aged 65 and above represent 57% of all rural veterans who are enrolled in the Veterans Health Administration (VHA; Department of Veterans Affairs, 2019a). These older adults often have multiple chronic conditions and aging-related issues that require care from multiple disciplines, including primary care, specialty care, mental health care, and coordinated health and social services; and yet, accessing these services at a health-care facility may require extensive travel. This article describes telehealth approaches by the VHA, including the Geriatric Research Education and Clinical Centers (GRECC) Connect clinical demonstration project, to increase access to geriatric care for aging veterans and family caregivers residing in rural areas.
Read more below.
CMS - Long-Term Care Nursing Homes Telehealth and Telemedicine Tool Kit
Intent of Toolkit: Under President Trump’s leadership to respond to the need to limit the spread of community COVID-19, the Centers for Medicare & Medicaid Services (CMS) has broadened access to Medicare telehealth services so that beneficiaries can receive a wider range of services from their doctors without having to travel to a healthcare facility. These policy changes build on the regulatory flexibilities granted under the President’s emergency declaration. CMS is expanding this benefit on a temporary and emergency basis under the 1135 waiver authority and Coronavirus Preparedness and Response Supplemental Appropriations Act. The benefits are part of the broader effort by CMS and the White House Task Force to ensure that all Americans – particularly those at high-risk of complications from the virus that causes the disease COVID-19, are aware of easy-to-use, accessible benefits that can help keep them healthy while helping to contain the community spread of this virus.
Get access to CMS's telehealth tool kit below.
Telemedicine in the Era of COVID-19
About once in a generation, a global pandemic emerges and wreaks havoc on a vulnerable world population. This is why most of us have limited personal experience with such events. The present outbreak of a coronavirus-associated acute respiratory disease called coronavirus disease 19 (COVID-19) is the third documented spillover of an animal coronavirus to humans that is causing a major epidemic in the last 2 decades. Recent outbreaks such as severe acute respiratory syndrome in 2003 and Middle East respiratory syndrome in 2012 were successfully confined to small regions of the planet. As such, they were of peripheral concern to allergists practicing in the United States because we and our patients were not exposed to them. Now that COVID-19 is affecting us and our patients directly, concerns about this novel emerging infection have gone, well. viral. It was only a matter of time until a global pandemic affected us, and our time has run out.
Read more of this editorial below.
Covid-19 and the Need for Health Care Reform
The Covid-19 pandemic has brought into sharp focus the need for health care reforms that promote universal access to affordable care. Although all aspects of U.S. health care will face incredible challenges in the coming months, the patchwork way we govern and pay for health care is unraveling in this time of crisis, leaving millions of people vulnerable and requiring swift, coordinated political action to ensure access to affordable care.
Read more of Dr. King's perspective below.
Securing the Safety Net and Protecting Public Health During a Pandemic
The coronavirus disease 2019 (COVID-19) has exposed gaps in the social safety net in the US. Medicaid, which covers 71 million individuals, has an important responsibility in addressing these gaps. Medicaid programs can fund unexpected health care services that other insurance plans may exclude and are thus well-positioned to ensure that vulnerable patients have access to important health care services and that hospitals and other health care organizations and clinicians are reimbursed for providing that care.
States can take several actions to waive federal or state requirements to accomplish the following goals: (1) improving prompt testing and treatment of patients with COVID-19, (2) mitigating the strain on the health care system and preserving the capacity of hospitals and health care practitioners, and (3) limiting transmission of COVID-19 by facilitating changes in how care is delivered. Through the series of actions outlined below, Medicaid programs should have a key role in protecting enrollees, supporting public health efforts to reduce the spread of the virus, and aiding the health care system to increase capacity.
Reach more of this perspective below.
Covid-19 and Health Care’s Digital Revolution
In the face of the Covid-19 outbreak, Americans are waking up to the limitations of their analogue health care system. It seems clear that we need an immediate digital revolution to face this crisis.
Click below to read this perspective.
Balancing health privacy, health information exchange, and research in the context of the COVID-19 pandemic
The novel coronavirus disease 2019 infection poses serious challenges to the healthcare system that are being addressed through the creation of new unique and advanced systems of care with disjointed care processes (eg, telehealth screening, drive-through specimen collection, remote testing, telehealth management). However, our current regulations on the flows of information for clinical care and research are antiquated and often conflict at the state and federal levels. We discuss proposed changes to privacy regulations such as the Health Insurance Portability and Accountability Act designed to let health information seamlessly and frictionlessly flow among the health entities that need to collaborate on treatment of patients and, also, allow it to flow to researchers trying to understand how to limit its impacts.
Click below to read more.
