Implementation best practices: Dealing with the complexity of AI
Implementation best practices: Dealing with the complexity of AI
Artificial intelligence is just as complex as it sounds. Successful deployment of the various technologies that are necessary for AI to work requires planning and strategy..
To help chief information officers and other IT professionals better understand these best practices for implementing AI at their health systems, hospitals, group practices and other provider organizations, we spoke with four experts in AI technologies who offered their advice for effective rollouts.
Best Practices
- Identifying use cases - By identifying use-cases and successes, you can help categorize vendors who have a proven track record of success while reducing the financial risk your healthcare organization takes on by purchasing an AI tool.
- The expected value - When it comes to implementing AI, there is no substitute for sound business principles. CIOs should apply the same rigor in the adoption of AI that they apply in the adoption of any other new technology. As CIOs pursue a portfolio of initiatives, it’s critical to work with partners who can introduce solutions to a variety of areas in the hospital or network.
- The operational state - A key must-have when implementing an AI system is a clear vision of an organization's operational state and business goals.
- Focus on outcomes - Set goals and make sure you have ways to benchmark the success of the AI solution – know how long it will take to see an outcome.
The full Healthcare IT News article can be viewed at this link.
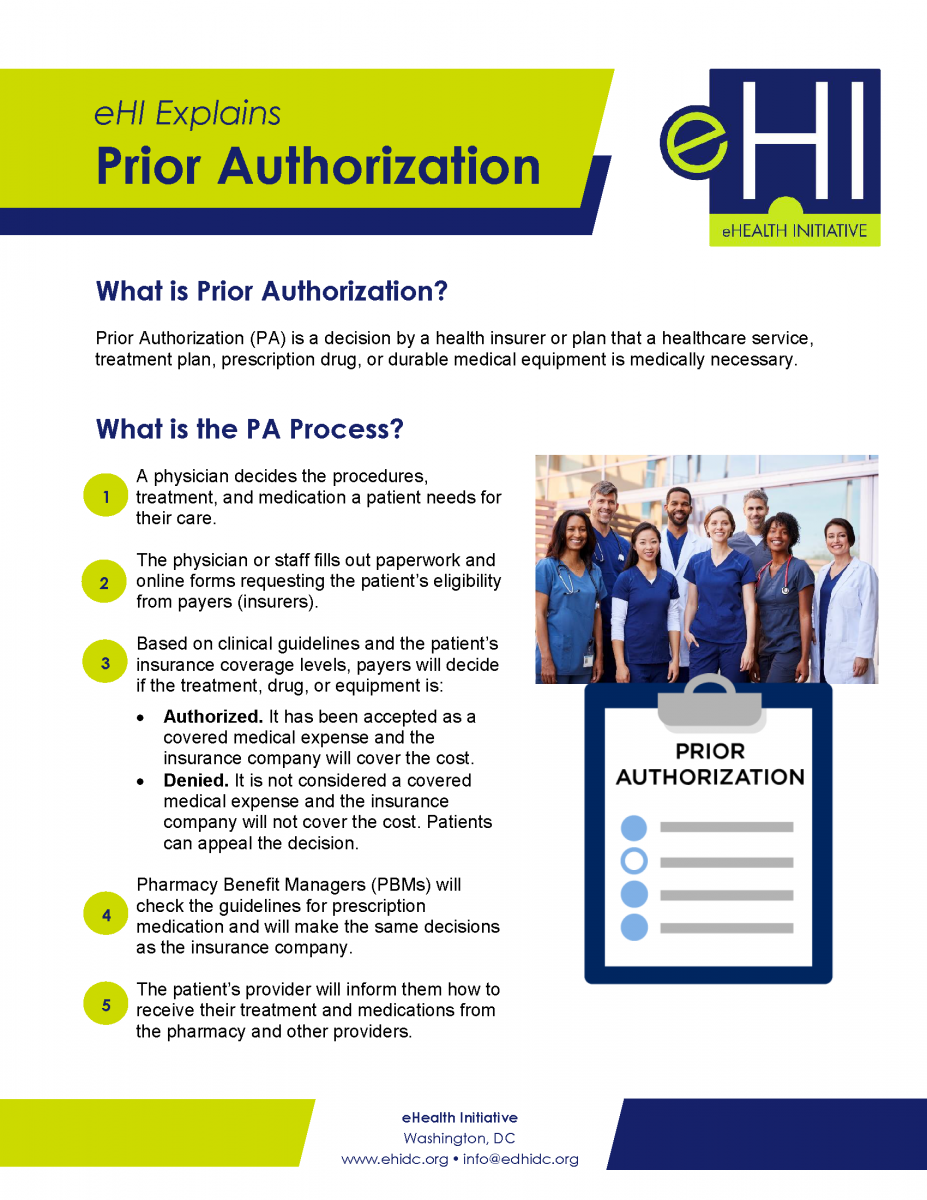
eHI Explains Prior Authorization
Prior Authorization is a decision by a health insurer or plan that a healthcare service, treatment plan, prescription drug, or durable medical equipment is medically necessary. This document gives a simple explanation of the Prior Authorization process and provides an overview of eHealth Initiative's Prior Authorization Project and considerations for improving Prior Authorization. Download the document below.
Considerations for Improving Prior Authorization Document
 In 2018 and 2019, eHealth Initiative (eHI) convened a series of prior authorization workshops with representatives from key stakeholder organizations across healthcare. The goal of the workshops was to establish a set of recommended practices to help improve the current prior authorization environment and to respond to the widespread challenges and dissatisfaction healthcare professionals have with prior authorization.
In 2018 and 2019, eHealth Initiative (eHI) convened a series of prior authorization workshops with representatives from key stakeholder organizations across healthcare. The goal of the workshops was to establish a set of recommended practices to help improve the current prior authorization environment and to respond to the widespread challenges and dissatisfaction healthcare professionals have with prior authorization.
United States healthcare spending grew to $3.5 trillion by the end of 2017, and approximately 1 in 3 dollars of those expenditures do not actually improve health. Experts estimate that about 30% of health spending is wasted on unnecessary services, excessive administrative costs, fraud, and other problems. Prior authorization is also meant to optimize patient outcomes and protect their safety. Healthcare payers utilize prior authorization to keep costs in check while reducing waste; error; and unnecessary procedures, treatments, and prescriptions.
The prior authorization process has, however, proved burdensome for healthcare professionals (clinicians, nurses, physicians, and others who provide care directly to patients) and can result in delayed or denied patient care. A recent American Medical Association (AMA) survey revealed that 86% of physician respondents feel that the burden associated with prior authorization in their office is either “high or extremely high” and that they and their staff spend an average of 14.9 hours each week to complete the prior authorization workload.
Download the full report below.
.
The Deadly Consequences Of Financial Incentives In Healthcare
The Deadly Consequences Of Financial Incentives In Healthcare
For decades, elite business schools have touted the benefits of financial incentives to motivate sales teams, factory workers and rising executives. Results are mixed.
In medicine, financial incentives rarely achieve their intended goals. It’s not because they don’t work. As I tell students at the Stanford Graduate School of Business, it’s because they work too well.
Monetary rewards always change doctor behavior, but rarely achieve the outcomes desired—something my predecessor learned the hard way when he tried to increase patient satisfaction.
This article also provides alternative best practices for improving patient satisfaction that avoids many of the discussed pitfalls of financial incentives.
Best Practices
- Transparency - Unblind the patient-satisfaction data for every physician and make the figures available for all to see. This allowed everyone to assess their own strengths and weaknesses.
- Education - We created educational programs to help physicians improve their satisfaction scores with personal coaching and development opportunities.
- Convenient access to care - We made it easier for doctors to satisfy patients by offering convenient access to care through technology.
The full Forbes article can be viewed at this link.
Improving Medical Device Security Beyond Patching, Traditional Tools
Improving Medical Device Security Beyond Patching, Traditional Tools
Medical device security was thrust into the spotlight in 2018, as the Food and Drug Administration continued to bolster its cybersecurity program. In fact, an August MedCrypt report found that since the FDA released its cybersecurity guidance in 2016, medical device vendors reported 400 percent more vulnerabilities per quarter.
The increase in disclosures is a sign of growing compliance and maturing security risk assessments – and the hope that healthcare is beginning to move the needle on device security.
Best Practices
- A unified strategy - Biomedical and IT should collaborate on device security.
- Monitor traffic - Watch traffic for any rogue communication.
- Partner with device manufacturers - Getting inside information on what devices should be doing can help identify compromised devices.
- Awareness - Appreciate and accept that different approaches are needed to secure medical devices.
The full Healthcare IT Security article can be viewed at this link.
Perspectives and Best Practices for Artificial Intelligence and Continuously Learning Systems in Healthcare
Perspectives and Best Practices for Artificial Intelligence and Continuously Learning Systems in Healthcare
Healthcare is often a late adopter when it comes to new techniques and technologies; this works to our advantage in the development of this paper as we relied on lessons learned from CLS in other industries to help guide the content of this paper. Appendix V includes a number of example use cases of AI in Healthcare and other industries.
This paper focuses on identifying unique attributes, constraints and potential best practices towards what might represent “good” development for Continuously Learning Systems (CLS) AI systems with applications ranging from pharmaceutical applications for new drug development and research to AI enabled smart medical devices. It should be noted that although the emphasis of this paper is on CLS, some of these issues are common to all AI products in healthcare.
The full paper can be downloaded below.
How to get started in quality improvement: Best Practices
How to get started in quality improvement: Best Practices
Quality improvement is a core component of many undergraduate and postgraduate curriculums. Numerous healthcare organisations, professional regulators, and policy makers recognise the benefits of training clinicians in quality improvement.
Engaging in quality improvement enables clinicians to acquire, assimilate, and apply important professional capabilities such as managing complexity and training in human factors. For clinical trainees, it is a chance to improve care; develop leadership, presentation, and time management skills to help their career development; and build relationships with colleagues in organisations that they have recently joined. For more experienced clinicians, it is an opportunity to address longstanding concerns about the way in which care processes and systems are delivered, and to strengthen their leadership for improvement skills.
The benefits to patients, clinicians, and healthcare providers of engaging in quality improvement are considerable, but there are many challenges involved in designing, delivering, and sustaining an improvement intervention. These range from persuading colleagues that there is a problem that needs to be tackled, through to keeping them engaged once the intervention is up and running as other clinical priorities compete for their attention. You are also likely to have competing priorities and will need support to make time for quality improvement. The organisational culture, such as the extent to which clinicians are able to question existing practice and try new ideas, also has an important bearing on the success of the intervention.
This article describes the skills, knowledge, and support needed to get started in quality improvement and deliver effective interventions.
Best Practices
- Recognize needed skills- Enthusiasm, optimism, curiosity, perseverance, relational skills, practical skills, managing complexity, time management, and enjoying the experience are all necessary to build quality improvement.
- Build your team- The first step is to recruit your improvement team. You need a blend of skills and perspectives in your team. Find a colleague experienced in quality improvement who is willing to mentor or supervise you.
- Identify a problem- Next, identify a problem collaboratively with your team. Use data to help with this. Take time to understand the contextual factors and what might be causing the problem.
- SMART framework- Next, develop your aim using the SMART framework: Specific (S), Measurable (M), Achievable (A), Realistic (R), and Timely (T). This allows you to assess the scale of the intervention and to pare it down if your original idea is too ambitious. Aligning your improvement aim with the priorities of the organisation where you work will help you to get management and executive support.
- Map stakeholders- Having done this, map those stakeholders who might be affected by your intervention and work out which ones you need to approach, and how to sell it to them.
- Find support- You need support from both your organisation and experienced colleagues to translate your skills into practice.
The full article can be downloaded below.
Press Release: Sonora Quest Laboratories and Beacon Biomedical Partner to Launch BeScreened - CRC, a Blood-Test for Colorectal Cancer Screening
TEMPE, Ariz. (Dec. 10, 2018) – Sonora Quest Laboratories, Arizona’s leading provider of diagnostic testing and information services, and Beacon Biomedical Inc., a Phoenix-based diagnostic laboratory focused on commercializing early detection cancer tests, have jointly announced the availability of Beacon’s new colorectal cancer screening blood test called BeScreened™-CRC. Under an exclusive partnership the test is now available directly to consumers without a doctor’s order through Sonora Quest’s My Lab ReQuest™, their self-ordered lab testing product which is available on-line and at all of Sonora Quest’s 70-plus patient service centers across Arizona. In the near future, Sonora Quest and Beacon Biomedical intend on offering BeScreened-CRC throughout their entire network, including primary healthcare providers.
Recognizing that many people are unable or unwilling to use existing screening tests, Beacon Biomedical developed BeScreened-CRC as a convenient alternative to enable early detection, improve healthcare outcomes and reduce costs. BeScreened-CRC is 94 percent accurate at detecting the likely presence or absence of colorectal cancer, even in its earliest stages. As a blood test, it has the potential to remove many of the barriers to screening due to the test’s simplicity and ease of adoption, and it can be collected at the same time as other blood tests with no special preparation needed.
Download the press release to read more!
Press Release: Sonora Quest Laboratories Partners with uMETHOD Health to Advance the Care of Chronic Diseases with Precision Medicine
Arizona’s leading diagnostic provider offers first artificial intelligence-based precision medicine platform for Alzheimer’s disease
TEMPE, Ariz. (November 1, 2018) – Sonora Quest Laboratories, Arizona’s leading provider of diagnostic testing and information services, has announced a partnership with uMETHOD Health, a health technology company offering the first platform for Alzheimer’s disease based on advanced artificial intelligence technology. Through the partnership, healthcare providers will have access to the RestoreU METHOD via Sonora Quest for their patients experiencing memory loss. The platform includes lab tests and individualized care plans to assess and minimize risk of developing Alzheimer’s, and to help slow the progress of the disease in its early stages.
Download the press release to read more!
Press Release: Sonora Quest Laboratories Partners with BaseHealth; Groundbreaking Analytics Platform Reveals Hidden Health Risks and Cost Saving Opportunities
TEMPE, Ariz. (Nov. 9, 2018) – Sonora Quest Laboratories, Arizona’s leading provider of diagnostic testing and information services, and BaseHealth, a predictive health analytics company that empowers health systems and Accountable Care Organizations (ACO’s) to proactively manage rising risk within populations, are collaborating to offer a pioneering analytics platform that identifies unknown risks in patient populations for improved outcomes and presents opportunities for cost savings for healthcare systems across the country.
Download the press release to read more.
